Parents notice everything. The open mouth while watching cartoons, the snore that rattles the baby monitor, the dry lips at breakfast. These are small clues that breathing habits might be drifting off course. Many families are turning to simple tools to retrain those habits, and one name crops up often: a gentle adhesive band that surrounds the lips and prompts the mouth to stay closed, encouraging the nose to do its job. Used thoughtfully, it can be a helpful part of building healthy breathing in growing children.
What it is and how it works
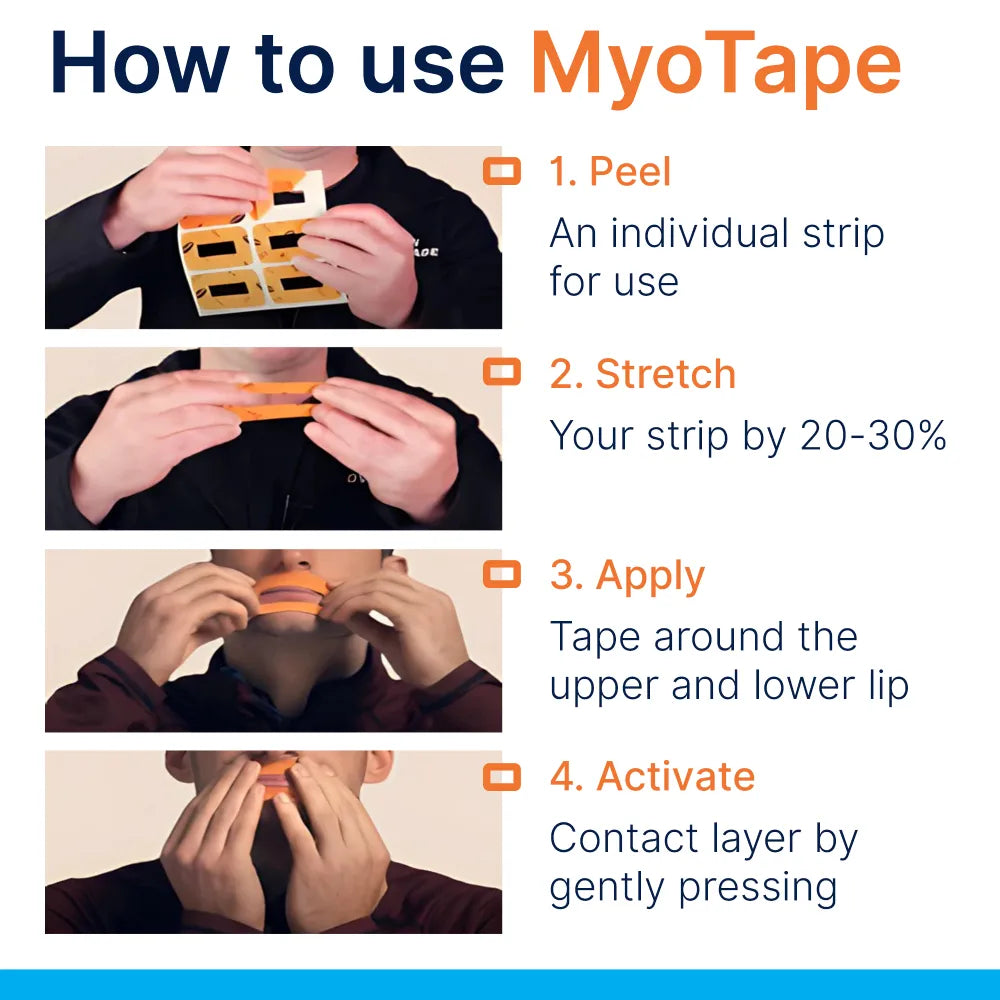
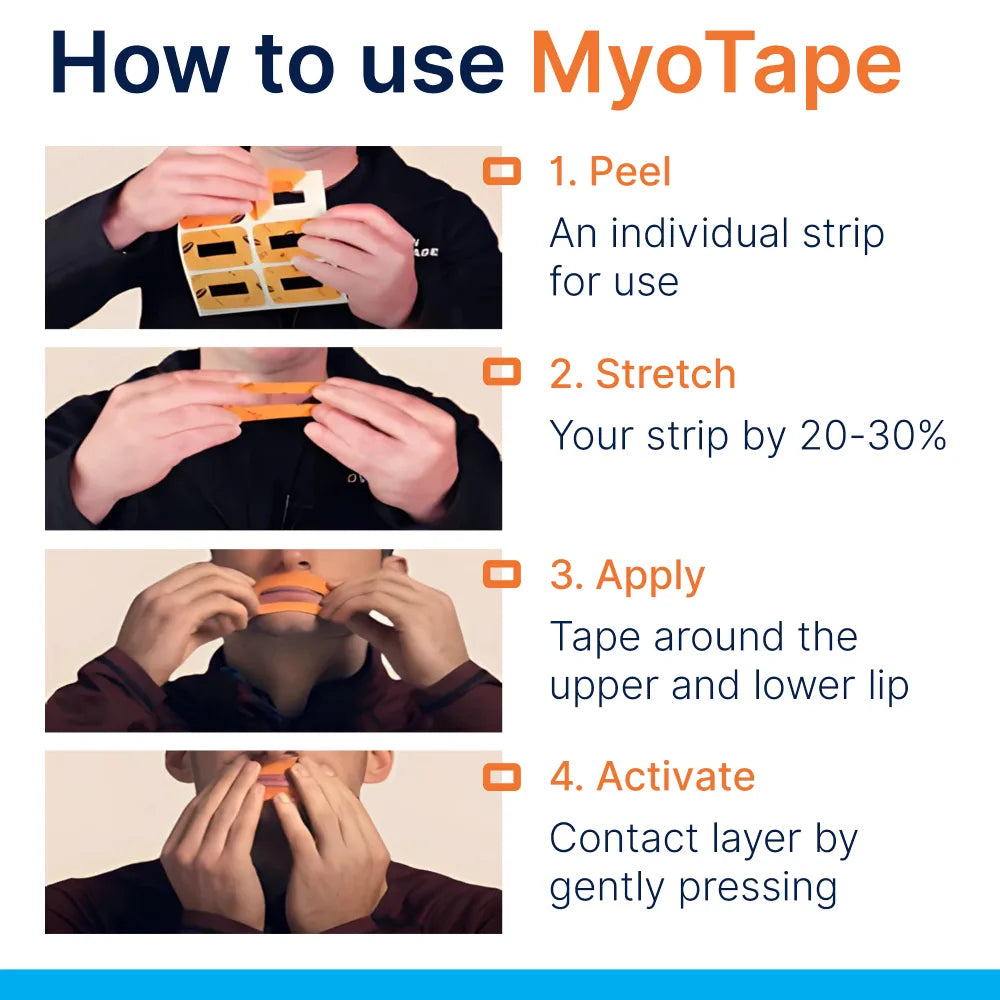
This taping approach is not about sealing lips shut. The kid-friendly version is a soft, stretchy strip that rests around the lips, leaving a free gap in the centre. The child can part the lips if they wish. The goal is to provide a tactile cue, a light reminder that the mouth prefers to rest closed while the nose takes the lead.
The effect is subtle. Over time, the brain links the sensation around the mouth with nasal breathing. That cue becomes a habit, especially when paired with myofunctional exercises, allergy support, and good sleep routines. Some families start during quiet reading, others during homework, then at night once confidence grows.
Why nasal breathing matters for growing children
Noses are built for breathing. They warm and filter air, conserve moisture and support nitric oxide production, which assists with oxygen delivery. The nose also helps regulate pressure in the upper airway. This matters during sleep when muscles relax.
For children, the pay-off can be wider than you might expect:
- Facial growth follows function. Lips together, teeth apart, tongue up on the palate is a well known rest posture that supports arch development and jaw guidance.
- Sleep is steadier when airflow is quiet and stable. Mouth breathing can dry tissues, irritate the throat and encourage snoring.
- Attention and mood can improve with better sleep. Teachers often notice changes in morning alertness once snoring settles.
- Dental health benefits from saliva staying where it should. A dry mouth tilts the balance toward plaque and cavities.
Paediatric dentists, ENTs and orofacial myologists often discuss nasal obstruction, enlarged adenoids, allergies and tongue posture in the same breath. Small adjustments in daily breathing can help reinforce the wider care plan that many children already follow.
What parents report when using kid-focused mouth taping
Every child is different, and no single product fixes everything. Even so, families commonly notice:
- Fewer overnight mouth openings and less drooling on pillows
- Quieter nights with reduced snoring
- Less morning dry mouth and sore throat
- A calmer bedtime routine once children get used to the cue
- Support for orthodontic aims when combined with expansion, myofunctional work or simple tongue posture training
- A nudge away from thumb or dummy comfort at night, as lips learn to rest together
Some parents also keep an eye on bedwetting, restless legs and night-time waking. Sleep quality affects many of these patterns, and steady nasal breathing can be one piece of the puzzle.
Safety first: who should and should not use it
Kid-friendly mouth taping is designed to be gentle, but it still deserves care and supervision. Keep these points front and centre:
- Age: generally suitable from around 4 years when a child understands the idea and can remove the tape independently. Use your judgement and always supervise.
- Never cover the entire mouth. The central lip gap must remain free.
- Avoid use with a blocked nose, cold, flu or active infection.
- Do not use in children with breathing disorders that are unstable, recent facial or oral surgery, severe skin conditions around the lips, or known adhesive sensitivities.
- Children with suspected sleep apnoea, enlarged tonsils or adenoids, frequent ear infections, marked nasal obstruction or craniofacial conditions need medical guidance first.
- Asthma that is well controlled is usually fine, but any flare-up warrants caution and a break.
- Do not use if there is nausea or a risk of vomiting.
- Always check that your child can remove the tape quickly and understands that they may open their mouth at any time.
One more safeguard: make nasal comfort the priority. If the nose is stuffy, treat that issue first with allergy care, saline rinses approved for kids, or a chat with an ENT or GP.
Getting started: a simple plan that works for busy families
Ease in. Make it a positive experiment rather than a strict rule.
- Check the nose
- Try the mirror test: ask your child to close their mouth, breathe through the nose for two minutes, and chatter about their day. If they struggle, address nasal health first.
- Clear routines at bedtime help. A warm shower, gentle saline spray and a calm story lower airway reactivity.
- Practise the posture
- Teach the rest position: tongue on the roof of the mouth, lips touching lightly, teeth apart. A quick rhyme helps kids remember.
- Try a single nasal inhale, slow nasal exhale, five times. Make it a game.
- Introduce the tape in the daytime
- Start with 10 to 20 minutes during screen time or reading.
- Explain the purpose in simple terms: this helps your nose do the breathing.
- Praise the effort, not perfection.
- Move to the first part of the night
- Use it for the first sleep cycle, then remove when you check on them.
- If all is calm for several nights, leave it for longer.
- Review weekly
- Keep notes on snoring, mouth opening, drool on the pillow, morning mood and energy.
- Adjust the plan with your dentist or therapist as needed.
Small steps help children buy in. The aim is consistency, not pressure.
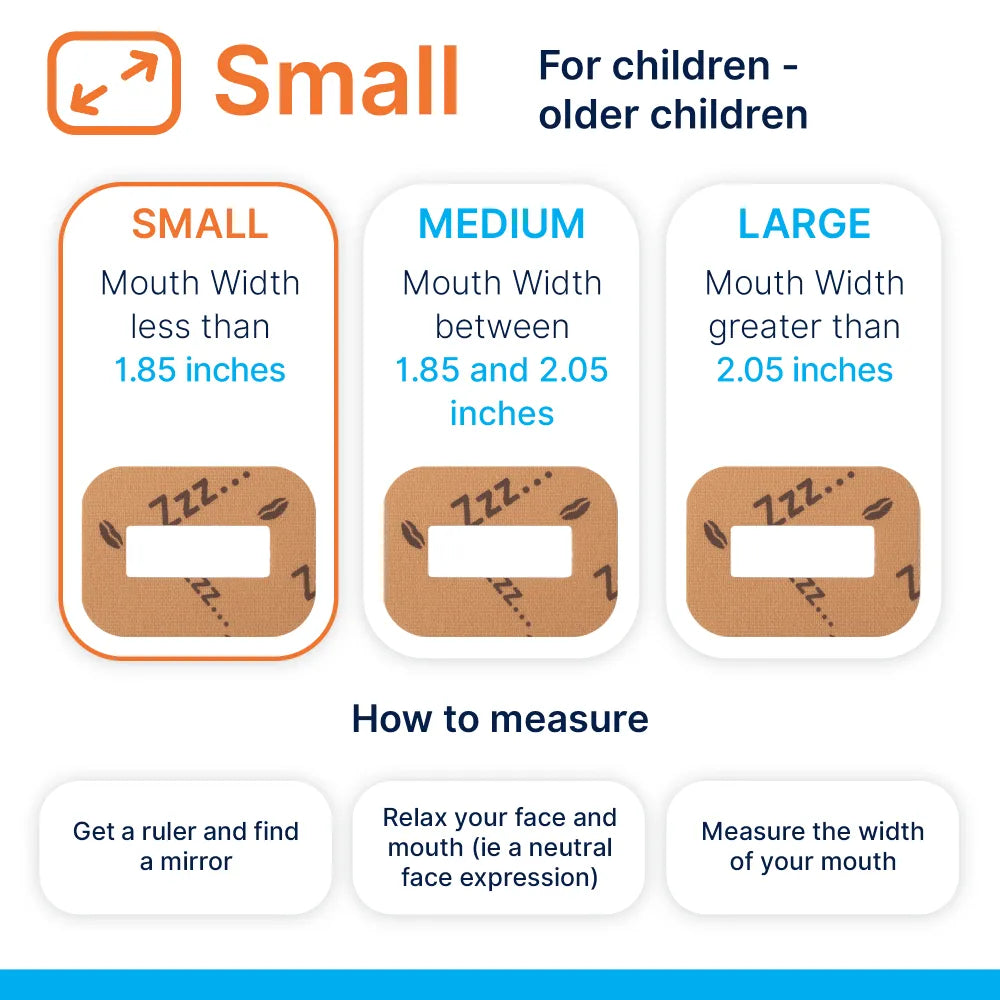
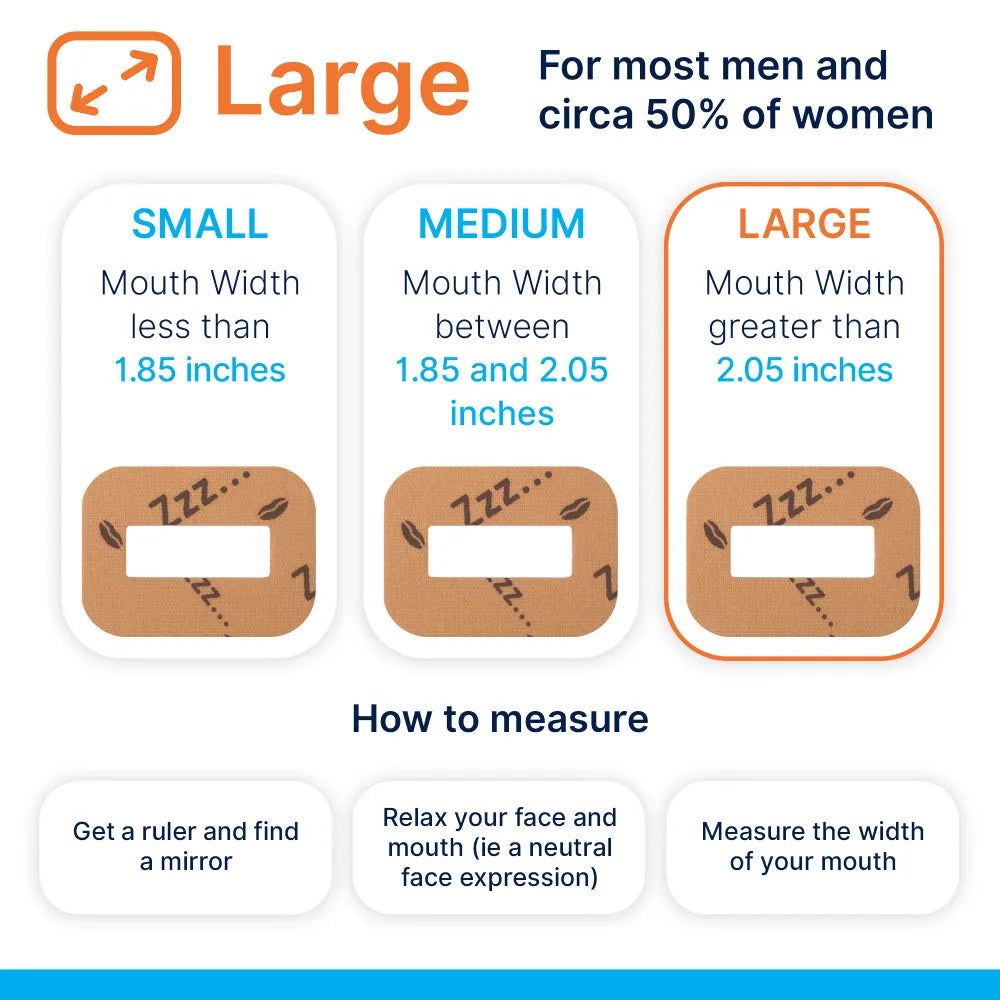
Choosing the right option
Parents often weigh up different tools that support nasal breathing. The key differences are shown below.
| Option | Placement | Can a child open their mouth | Speech and sipping water | Skin contact area | Typical comfort | Reuse |
|---|---|---|---|---|---|---|
| Around-the-mouth elastic tape designed for kids | Surrounds lips with central gap | Yes, lips can part | Yes, short phrases and small sips possible | Low to moderate | Soft and stretchy | Single use |
| Lip tape that seals lips | Directly over lips | Not easily | No | Moderate | Can feel restrictive | Single use |
| Chin strap | Wraps under chin and over head | Mouth often still opens | Muffled | Low | Varies, may slip | Reusable |
| No product, cue-based training only | None | Yes | Yes | None | No skin contact | Not applicable |
Kid-focused designs with a central opening tend to be better tolerated, especially during the learning phase. They give a cue without trapping the lips and allow speech if needed.
Integrating with orthodontics and myofunctional care
Healthy breathing habits make orthodontic treatment more stable. If a child sleeps with an open mouth after expansion, relapse pressure builds. If the tongue rests low and forward, arches narrow over time. Encouraging nasal breathing and good tongue posture reduces those headwinds.
Helpful additions to consider:
- A daily chew of textured foods to build jaw stamina, when appropriate for age and safety
- Lip seal games, balloon-blowing and gentle nasal breathing drills set by an orofacial myologist
- Allergy care and nasal hygiene habits that keep the nose calm
- Addressing habits like thumb sucking or dummy use that keep the mouth open
- Posture awareness for head and neck, since forward head posture can affect the airway
Work as a team: parent, child, dentist or orthodontist, and therapist. Each brings part of the solution.
Myths and worries that often arise
Taping a child’s mouth sounds alarming to some people at first glance. Reasonable questions deserve clear answers.
- They cannot breathe: designs for children leave a central gap and aim to encourage nasal priority. The child can open the lips and remove the strip. Parents should supervise and teach that autonomy explicitly.
- It forces a result rather than training a habit: the gentle ring acts like a band reminder. It cues the brain to keep the lips together without heavy pressure.
- Adhesives will harm the skin: quality products use skin-friendly adhesives. Even so, a patch test on the forearm is sensible. Apply to clean, dry skin and avoid if there is any irritation.
- It replaces proper medical care: it does not. Think of it as a small support that sits alongside treatment from ENTs, dentists, speech and myofunctional therapists.
Signs to pause and seek help
Stay responsive to how your child is doing. Stop using the tape and speak with a professional if you notice:
- Persistent or loud snoring, gasping, or laboured breathing at night
- Frequent waking, night terrors or sleepwalking that start after taping
- Panic or distress around the tape even after slow introduction
- Rashes, soreness or broken skin around the lips
- Ongoing nasal blockage despite good care
- Daytime sleepiness, behavioural changes or learning dips that worry you
These signs may point to airway obstruction, sleep disordered breathing or other issues that need proper assessment.
Making it child friendly
Success grows from comfort and routine. A few clever tweaks help:
- Turn it into a choice with stickers or a simple chart. Children like to track their streaks.
- Put the tape on after the story, not before. Calm first, cue second.
- Keep a water bottle by the bed. A small sip is fine if needed.
- Use a dim nightlight for reassurance during the first week.
- Pair it with a favourite soft toy to signal sleep time.
If a child resists, scale back to two minutes while reading. Build up slowly again.
What does progress look like
Parents describe a pattern that often follows predictable stages:
- Week 1: curiosity, a bit of fidgeting, occasional removal during sleep
- Week 2: longer stretches of nasal breathing, fewer removals, less drool
- Week 3 to 4: quiet nights more often than not, less morning dryness, brighter mornings
Track change with a simple scorecard:
- Snoring scale from 0 to 3
- Drool spots on the pillow, yes or no
- Waking events counted by the baby monitor
- Morning mouth dryness, yes or no
- Teacher feedback on attention and energy
Small wins add up. Photographs of restful lip seal during sleep can be surprisingly motivating for older children.
Practical care and skin tips
Good skin care keeps the routine comfortable.
- Apply on clean, dry skin. Oils and lip balms reduce adhesion and can irritate when trapped.
- Warm the strip between fingers for a second before placing. Gentle heat improves stick.
- Remove slowly from one corner while supporting the skin with the other hand.
- If skin is sensitive, rotate placement slightly to avoid the same spot every night.
- Store in a cool, dry spot and keep the pack sealed.
If redness appears, pause and reassess. A barrier gel or alternative adhesive may be needed after checking with a pharmacist.
Working with professionals
Collaboration gives better results. The right partners include:
- Paediatric dentist or orthodontist to evaluate jaw growth, crowding and bite
- ENT for nasal airway, adenoids, tonsils and allergy plans
- Speech and myofunctional therapists for tongue posture, chewing, swallowing and lip seal training
- GP or paediatrician to coordinate care if sleep or behaviour concerns persist
Bring notes and your weekly scorecard to appointments. Clear information speeds up decision making.
Frequently asked questions
Is it safe to use every night?
- Many families do, once tolerance is established and professionals are happy with the plan. Always supervise and reassess during colds or flare-ups.
What if my child needs to cough or speak?
- The central opening allows the lips to part. Teach your child that they can remove the strip at any time if uncomfortable.
Will it fix crooked teeth?
- It is not an orthodontic treatment. It supports the conditions that help orthodontic work hold its gains, particularly when tied in with good tongue posture and nasal health.
How long before I notice anything?
- Many parents notice changes in the first two to three weeks. Keep tracking and adjust the plan if progress stalls.
What if my child has allergies?
- Manage allergies first with your clinician. When the nose is comfortable, training nasal breathing is far more successful.
Does it help with bedwetting?
- Sleep quality and nasal breathing can influence night-time bladder control for some children. Results vary, and a continence plan may be needed alongside any breathing work.
A short checklist to print and keep on the fridge
- My child can breathe comfortably through the nose for two minutes at rest
- We practised tongue up, lips closed, teeth apart today
- Nasal rinse or saline used before bed if needed
- Tape applied around, not over, the lips
- Supervision in place for the first hours of sleep
- Morning notes recorded: snoring, drool, mood, dry mouth
- Break plan ready for colds, flare-ups or skin irritation
- Next review date with dentist or therapist marked on the calendar
Healthy breathing is a daily habit that pays dividends in sleep, growth and confidence. With patience, clear safety rules and support from the right clinicians, a simple cue around the lips can help many children find their nasal rhythm again.













0 comments