Parents often hear about taping methods that guide children toward nasal breathing during sleep and wonder if this could be a simple fix for snoring, mouth breathing or restless nights. The idea sounds straightforward. Encourage the lips to stay together, prompt nose breathing, and help the body settle. Reality is more nuanced, and safety sits at the centre of the decision.
This piece brings together what is known about mouth taping products that sit around the lips, how they differ from full-coverage tape, where the risks may lie, and the steps parents can take to make an informed choice.
What it is and how it is meant to work
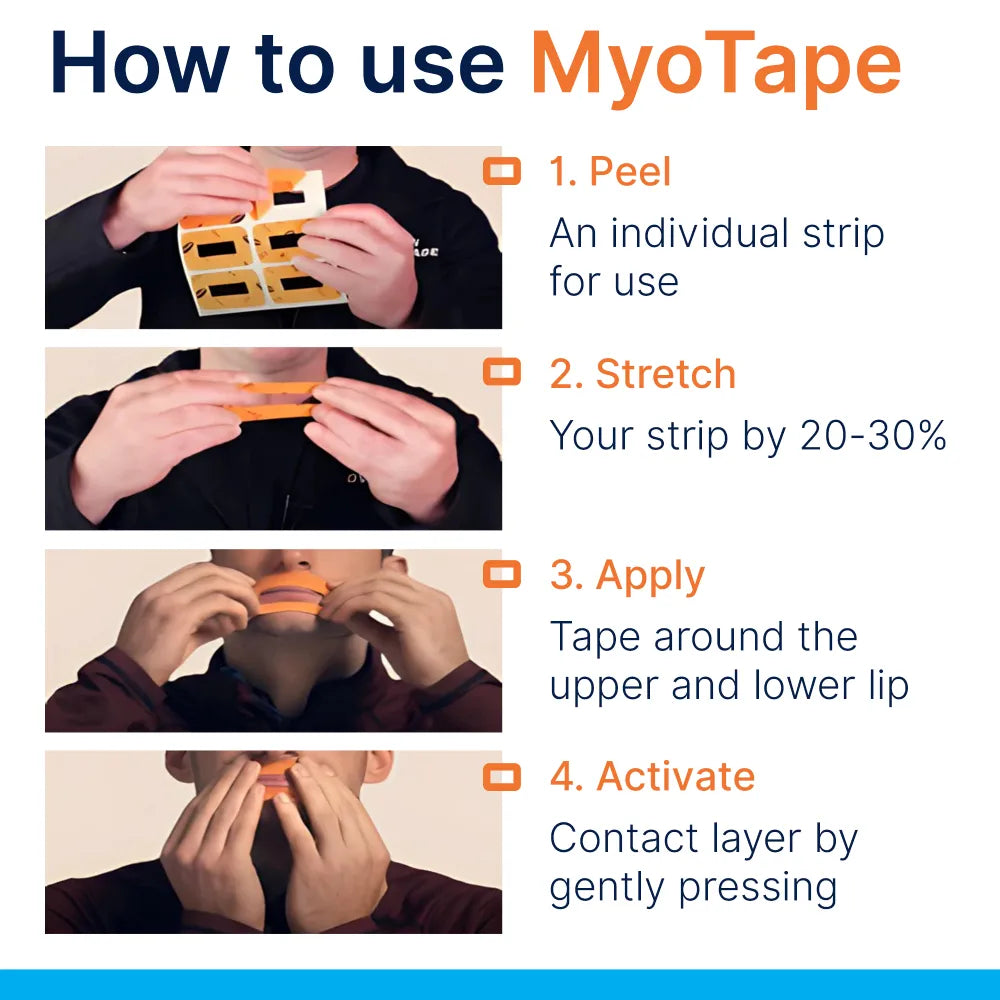
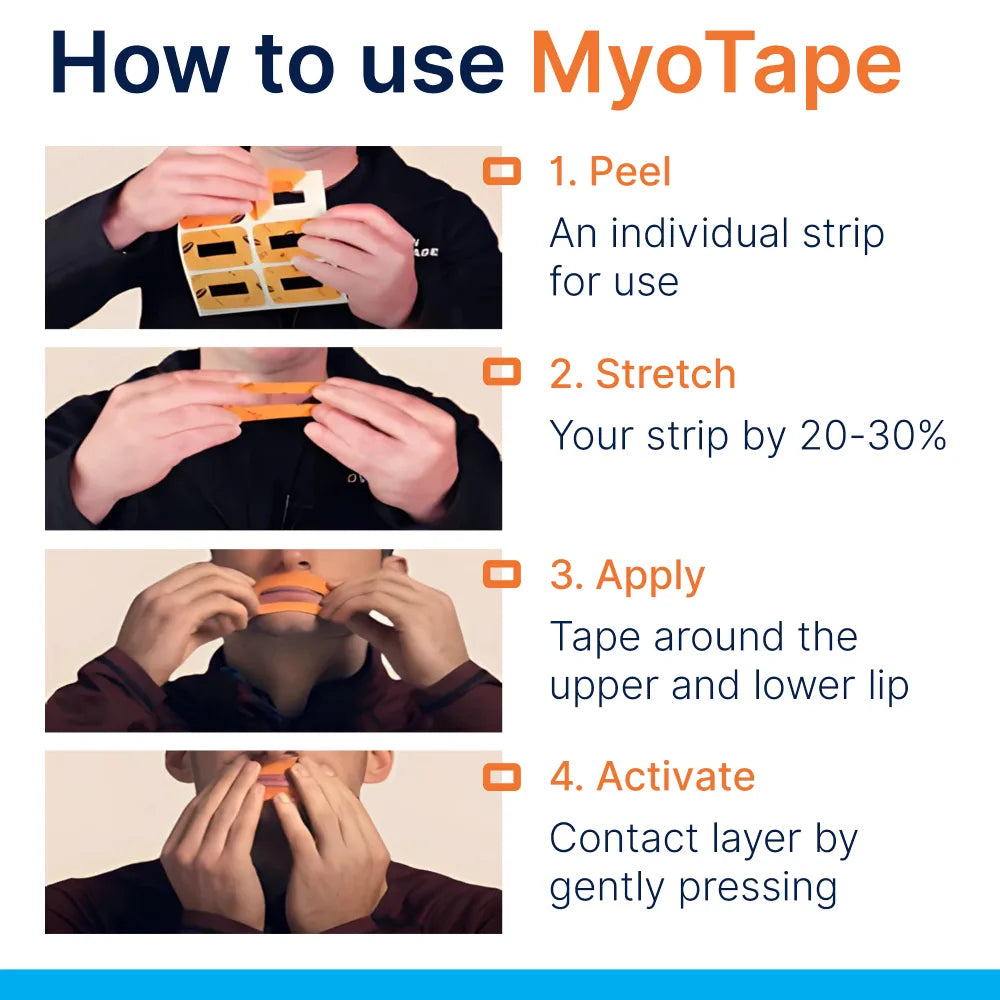
Several brands sell elastic adhesive strips designed to sit around the mouth, not across it. The material draws the lips inward, reminding the child to keep a gentle lip seal. Air can still pass through the centre. That design feature separates these products from DIY methods that block the lips completely.
Why does this matter? Habitual nose breathing influences facial growth, tongue posture and the way the airway develops. When the nose is used, air is filtered, warmed and humidified. Nitric oxide from the sinuses supports oxygen uptake. These points are well established in respiratory medicine, orthodontics and sleep health.
Tape alone does not cure an airway problem. The intention is that it can support better habits during sleep, and sometimes during quiet activities in the day. Some families use it as a training aid alongside myofunctional therapy, orthodontic care or allergy management.
Safety in brief
- The children’s versions are designed to allow a small gap for airflow and should not occlude the mouth
- Use is not advised for very young children
- Screening for nasal blockage matters more than any brand choice
- Night-time supervision and staged introduction reduce risk
- Evidence for kids is limited, so medical input is wise if snoring, pauses in breathing or daytime symptoms are present
Age guidance and supervision
Manufacturers of around-the-lips tape typically offer a children’s size and state a lower age limit. Four years is a common cut-off. Below that age, cooperation and communication during the night are less reliable, and adhesive contact with sensitive skin can be problematic.
Points to apply at home:
- Do not use with infants or toddlers
- Introduce during quiet daytime tasks first, when you can watch closely
- Night use calls for a parent nearby, especially in the early phase
- If a child is anxious about the idea, do not push it
The difference between around-the-lips tape and mouth covering
Two phrases often get mixed up. Mouth taping as a headline can mean anything from a strip straight across the lips to an elastic frame that hugs the skin like a soft ring. These are not equal in risk.
- Around-the-lips tape: leaves a clear central gap, relies on elastic tension to cue the lips to meet
- Across-the-mouth tape: seals the lips completely and blocks the mouth
Parents who are looking at safety should avoid any method that seals the mouth. A product that keeps the lips close without blocking airflow is less risky, though still not suitable for every child.
Situations where parents should not use it
Some scenarios call for a firm no. If any of the following apply, skip tape and speak to a clinician.
- Known or suspected obstructive sleep apnoea, especially if there are pauses in breathing, gasping, bedwetting or marked daytime fatigue
- Significant nasal congestion from allergy, a cold, sinus infection or enlarged adenoids or tonsils
- Frequent vomiting or reflux at night
- Asthma that is not fully controlled, recent chest infection or chronic lung disease
- Night-time seizures or epilepsy
- Developmental conditions or anxiety that would make removal difficult
- Skin conditions on or around the lips, or allergy to adhesives
- Structural nasal problems that reduce airflow, such as a severe deviated septum
If any doubt remains, err on the side of caution and seek an assessment first. Mouth breathing in children can reflect an airway problem that needs treatment.
What the research shows, and what it does not
- Adult data: Small trials have shown that keeping the mouth closed at night may reduce snoring in some adults with mild issues. Results vary, and study quality is mixed.
- Children: Direct evidence on around-the-lips tape for safety and effectiveness in children is sparse. There is better evidence for myofunctional therapy, allergy control, expansion appliances in orthodontics and adenotonsil surgery when indicated.
- Physiology: Encouraging nasal breathing can support better carbon dioxide tolerance, improved airway conditioning and a more stable tongue posture. These points support the rationale, but do not replace trials in paediatrics.
The takeaway is straight. Tape may help habit formation for selected children who can breathe comfortably through the nose, but it should sit behind medical assessment when symptoms suggest airway disease.
A simple screening routine at home
Before any overnight trial, run through a practical checklist over several days.
- Daytime nasal breathing check
- Ask your child to sit upright and breathe gently through the nose for five minutes while reading or drawing
- Watch for open-mouth periods, effort, flaring of the nostrils or complaints of “stuffy nose”
- If the child struggles, address nasal hygiene and allergy first, or seek advice
- Light lip cue without adhesive
- Try a soft reminder: “tongue to the spot” behind the upper teeth and lips together
- If the child can maintain a relaxed seal without stress, that is a positive sign
- Skin test
- Place a small piece of the adhesive on the inner forearm for 30 minutes
- Look for redness, itching or rash in the next 24 hours
- Trial while awake
- Apply the tape during a calm activity for 10 to 20 minutes
- Reinforce that removal is allowed at any time
- Watch for panic, coughing, or the urge to mouth breathe
If any step raises concern, pause and rethink the plan.
How to introduce it safely
The aim is to keep the process calm and reversible.
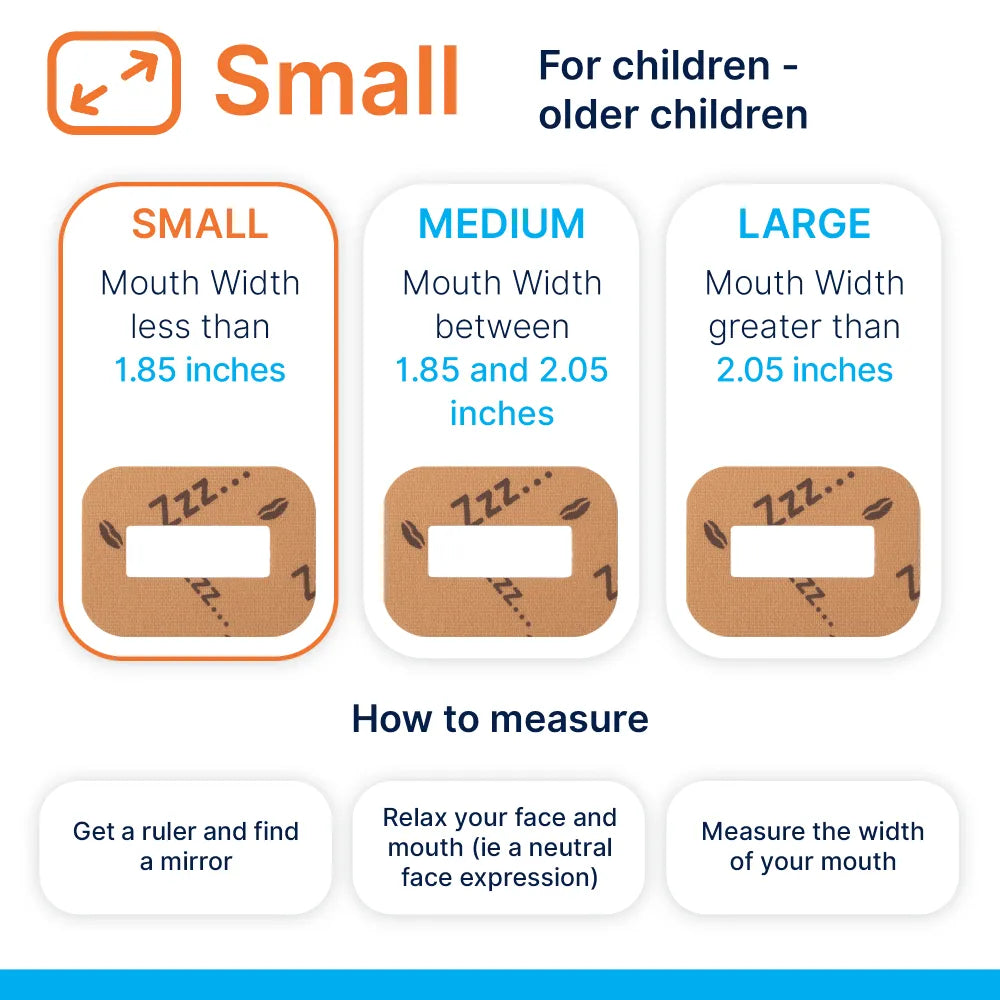
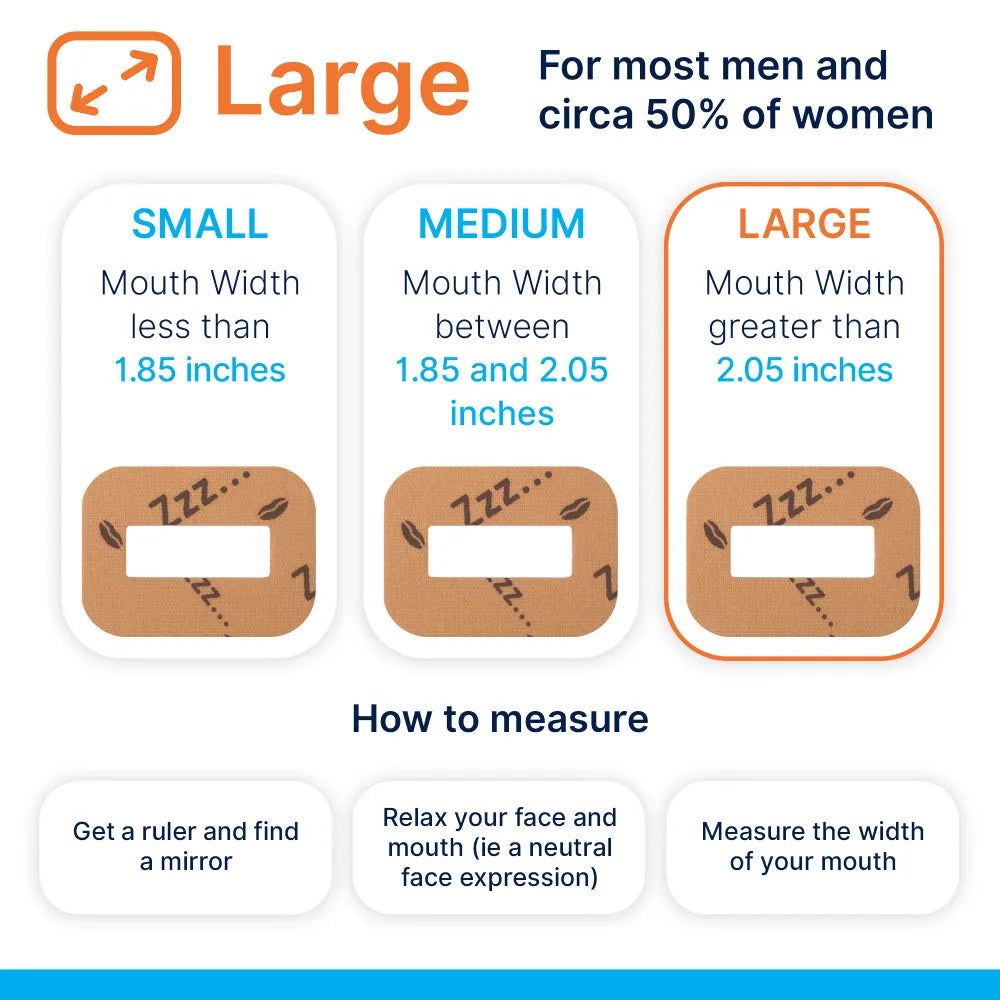
- Choose a children’s size that fits around the mouth without stretching the skin
- Apply after the bedtime routine once the nose is clear and the child is settled
- Keep a night light on so the child can wake and remove the tape easily
- Place the tape so a clear central gap remains for emergency mouth breathing
- Start with short naps when a parent can supervise, then consider night-time use
Teach removal. The child should know they can peel it off quickly, with no penalty or fuss.
Monitoring sleep and daytime signals
Over two to four weeks, watch for changes. Small, steady gains are more valuable than one dramatic night.
Positive signs:
- Quieter breathing and fewer mouth-open moments when checked during the night
- Waking with a moist mouth rather than dryness
- Less restless sleep and fewer sheet tangles
- Improved morning mood and easier focus at school
Warning signs:
- Any episode of choking, gasping, or clear distress
- Nosebleeds or worsening nasal blockage
- Rash or soreness around the lips
- New bedwetting or headaches on waking
- No change in snoring, or worsening snoring
If mixed signals appear, stop the tape and consult a clinician. A referral to an ENT specialist, orthodontist or sleep clinic may be the next step.
Practical tips to keep the nose clear
Several low-tech habits can make a real difference to nasal patency.
- Saline rinse before bed during allergy seasons
- Shower in the evening to remove pollen from hair and skin
- Dust mite covers for pillows and regular hot washes for bedding
- Pet-free bedrooms
- Humidifier if air is very dry, aiming for moderate humidity
A paediatrician or GP can advise on nasal steroid sprays, antihistamines or other treatments when allergies are active.
Where this fits among other options
Parents weigh tape alongside other tools. Each has a place, and each has limits.
- Myofunctional therapy trains tongue posture, nasal breathing and correct swallowing patterns
- Orthodontic expansion may widen narrow palates and improve nasal airflow
- ENT care addresses adenoids, tonsils and nasal obstruction
- Nasal dilators can ease airflow at the nostrils
- Chin straps lift the jaw but do not promote nasal airway quality and can be uncomfortable
- Habit coaching during the day is often overlooked and can be effective
Comparing common approaches
| Method | What it does | Can kids use? | Pros | Cautions |
|---|---|---|---|---|
| Around-the-lips tape | Encourages gentle lip seal, leaves central gap | Yes, with age limits and supervision | Reminds without full blockage, easy to remove | Not for nasal obstruction or anxiety, skin irritation possible |
| Full mouth-covering tape | Seals lips completely | No | None for children | Blocks emergency breathing, higher risk profile |
| Nasal dilator (external) | Lifts nasal valve for easier flow | Sometimes, check sizing | Non-invasive, no mouth contact | Limited effect with deeper nasal issues |
| Chin strap | Supports jaw closure | Rarely recommended in kids | Simple concept | Can restrict jaw motion, not a nasal solution |
| Myofunctional therapy | Trains tongue and breathing habits | Yes | Targets root habits, daytime gains | Needs daily practice, requires specialist guidance |
| Orthodontic expansion | Widens palate and nasal floor | Yes, when indicated | Structural change, can improve airflow | Requires specialist care and monitoring |
Common questions from parents
Is it safe if my child sometimes has a cold?
- No. Skip tape during any cold or sinus infection. Children should be able to breathe comfortably through the nose at rest before using any adhesive around the lips.
Could my child vomit at night and aspirate?
- If vomiting is likely, do not use the product. The risk of aspiration is the key concern many clinicians raise with any mouth restriction.
What about skin reactions?
- Hypoallergenic adhesives reduce risk but do not remove it. Patch test first and check the skin each morning.
Can this replace treatment for adenoids or enlarged tonsils?
- No. If a specialist has identified obstruction, address that directly. Tape does not correct anatomical blockage.
Does it stop snoring?
- Some children who mouth breathe lightly may snore less when their lips are gently trained to stay closed. If snoring is frequent or loud, seek a proper assessment for sleep-disordered breathing before trying tape.
What if my child has braces?
- Around-the-lips designs do not touch the brackets. If there is mouth dryness, wax irritation, or discomfort, speak to your orthodontist first.
Talking with clinicians
Bring clear observations to the appointment. Short notes help the discussion and speed the right referral.
Helpful items to share:
- A two-week sleep diary with typical bedtimes, wake-ups and any snoring or mouth breathing
- Daytime symptoms, including mouth dryness on waking, nasal congestion patterns and school focus
- A brief family history of allergy, asthma or sleep apnoea
- Photos or short recordings of sleep sounds, if the clinician agrees to review them
Ask direct questions. Would my child benefit more from allergy treatment, nasal steroid trial, myofunctional therapy or orthodontic expansion? Is a sleep study warranted? Where does a training aid fit within that plan?
Building good breathing habits in the day
If a child cannot maintain nasal breathing during calm activities, night-time training will be frustrating. Small daily routines can shift habits.
- “Tongue to the spot” cue during reading or homework
- Lips together, teeth apart, relaxed jaw
- Gentle nasal breathing during screen time, with regular posture breaks
- Short nose-breathing walks, focusing on quiet steps and closed lips
Make it light. Five minutes, twice a day, works better than long sessions that become a chore.
Signals that a different path is needed
Some patterns suggest that a tape-based approach is not the right tool right now.
- Persistent mouth breathing despite clear nose and daytime practice
- Behavioural changes, poor growth or very enlarged tonsils on inspection
- Craniofacial features linked to airway issues, such as a high narrow palate and crowded teeth
- Recurrent ear infections or chronic nasal speech
A combined plan with ENT, orthodontics and therapy may serve the child better than a training aid alone.
Putting safety first without losing momentum
Parents often want to act quickly when sleep is unsettled. Quick wins are great, yet the safest progress comes from a staged plan.
- Check nasal comfort and clear any obvious obstruction
- Practise gentle lip seal in the day without adhesives
- Patch test the skin
- Supervised short trials while awake
- Consider night-time use only when the child is calm, cooperative and breathing well through the nose
- Keep a log and be ready to stop if warning signs appear
Care, patience and the right clinical help can transform sleep and breathing in a way that lasts.
When a product might be a good fit
There is a subset of children who may do well with a gentle cue around the lips.
- Age four and up
- No nasal blockage at rest
- No history of sleep apnoea or significant snoring
- Calm temperament with good insight and willingness to try
- Supportive family, with a parent close by during early nights
In this group, the goal is not to tape forever. The ideal outcome is that nasal breathing becomes natural, and the tape fades away.
Signs of progress worth tracking
Keep the records simple and visual. A one-page chart over a month can show patterns that memory misses.
- Nights per week with quiet nose breathing
- Morning reports of dry mouth or thirst
- Frequency and loudness of snoring, if present at baseline
- Daytime focus and energy level
- Skin status around the lips
After three to four weeks, review the chart and decide. Continue, pause, or shift to a different approach.
Final pointers for parents
- Treat any form of mouth taping with respect, not as a quick trick
- Prefer around-the-lips designs that allow airflow
- Never use during illness, congestion or vomiting risk
- Involve a clinician if symptoms are moderate to severe or persistent
- Aim for habit change, not dependency on a product
The safest path is a thoughtful one. A child who breathes well through the nose during the day, sleeps comfortably, and wakes refreshed is the real target. If a tool helps you move in that direction, and it passes sensible safety checks, it may have a place. If not, the right help exists, and early action pays off.













0 comments