Many parents notice their child’s lips resting apart during the day or at night and wonder if it matters. It does. Mouth posture influences breathing, sleep, oral health and even facial growth. If you have heard about taping products designed for children and you are trying to separate hype from helpful, this guide walks through what they are, how they might help, and how to use them with care.
The aim is simple: help a child return to easy, reliable nasal breathing and a calm closed-lip rest posture. Everything else supports that goal.
Why an open mouth matters
The nose filters, warms and humidifies air. It also supports nitric oxide production in the nasal passages, which helps keep airways open. When a child habitually breathes through the mouth, those advantages are lost. The result is a dry mouth, a higher risk of tooth decay, irritated gums and a greater load on the throat.
Facial growth is guided by function. A relaxed tongue to the palate, lips together and breathing through the nose encourages a wider upper jaw and more space for teeth and the airway. A low tongue and open lips can nudge growth in the opposite direction, often showing up as a narrow palate, dental crowding or a longer face pattern over time.
Sleep quality can suffer too. Mouth breathing is linked with snoring, fragmented sleep and restless nights. Tired children are not always sleepy; many show hyperactivity, emotional swings and poor attention. Addressing breathing habits can lead to calmer days and better school performance.
None of this means families should panic. It means there is real value in helping children build a healthy lip seal and nasal breathing pattern.
What these tapes are and how they work
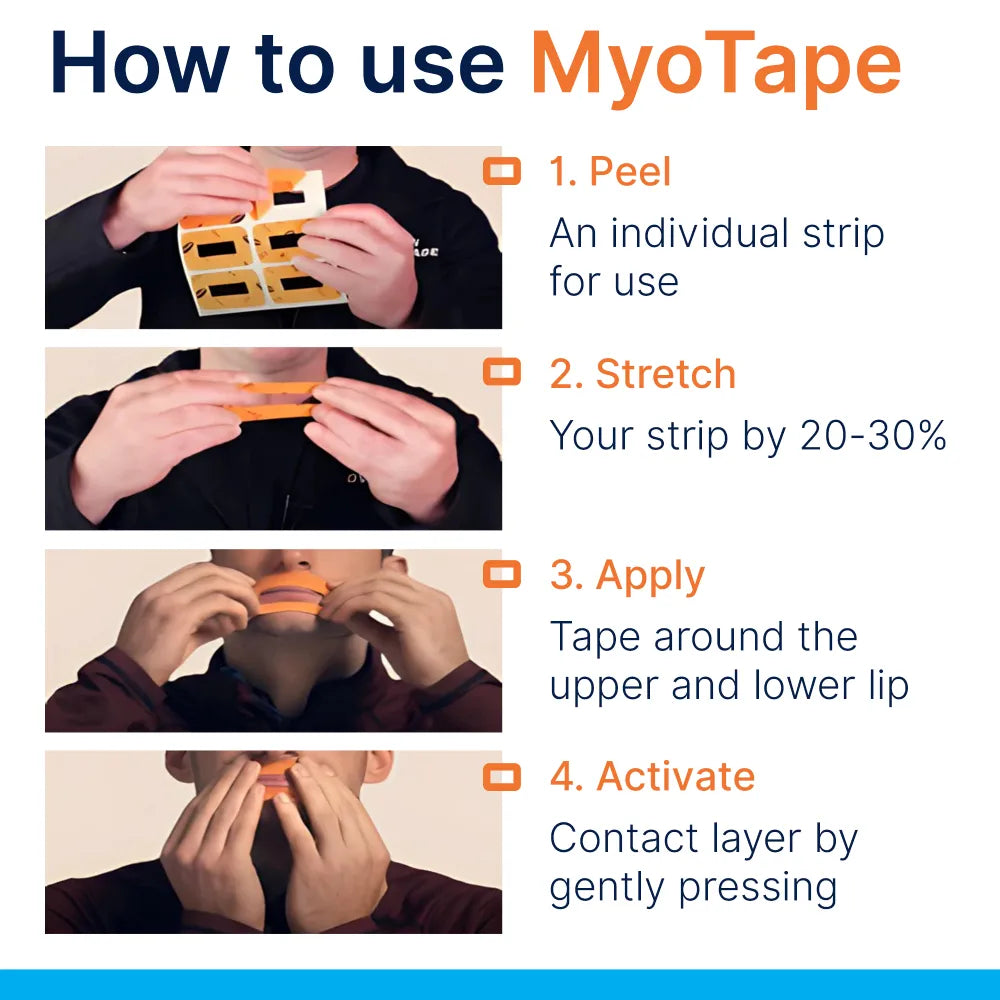
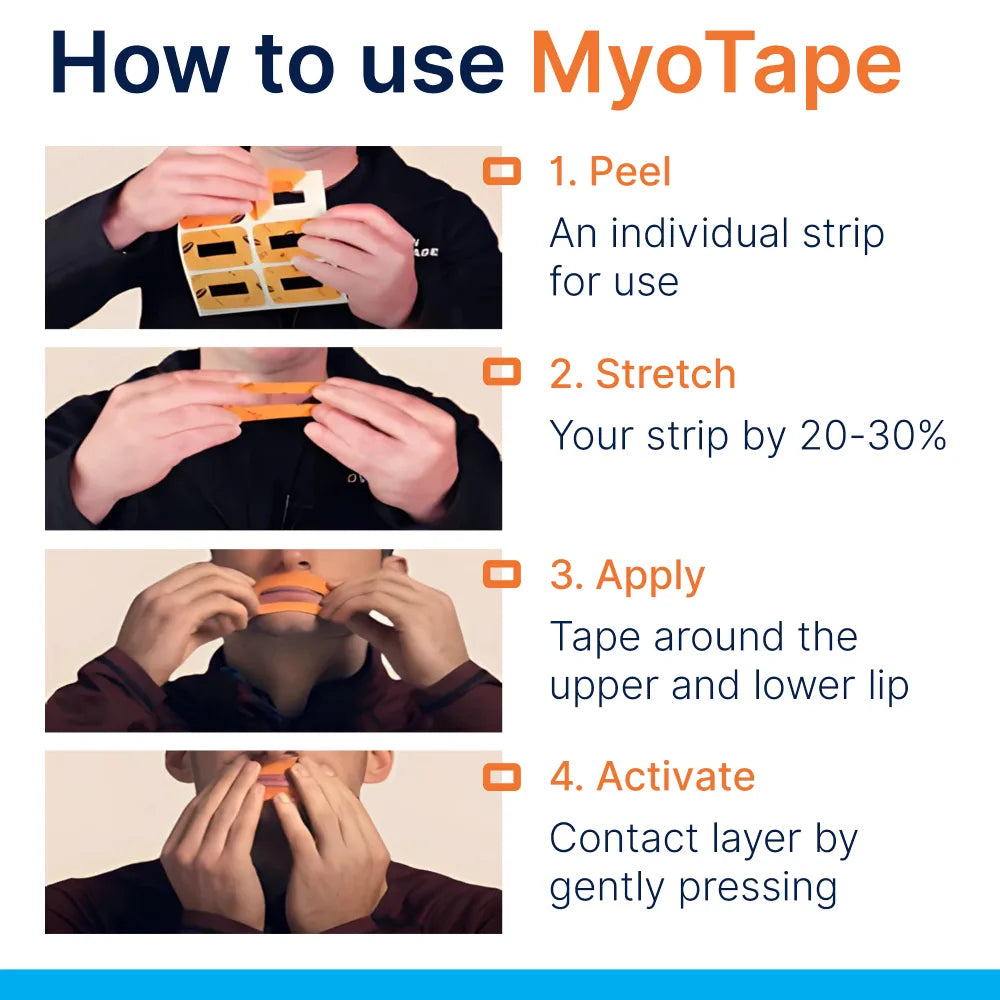
Children’s lip tapes sit around the mouth rather than across it. They are made from soft, elastic fabric with a gentle adhesive. The centre is open, so the lips are not physically stuck shut. The stretching band draws the lips together and reminds the child to keep the mouth closed, while still allowing a quick sip of air if needed.
Think of it as a sensory cue combined with a light mechanical nudge. It helps break the habit of lips drifting apart, and it gives the upper and lower lips a chance to strengthen their natural seal.
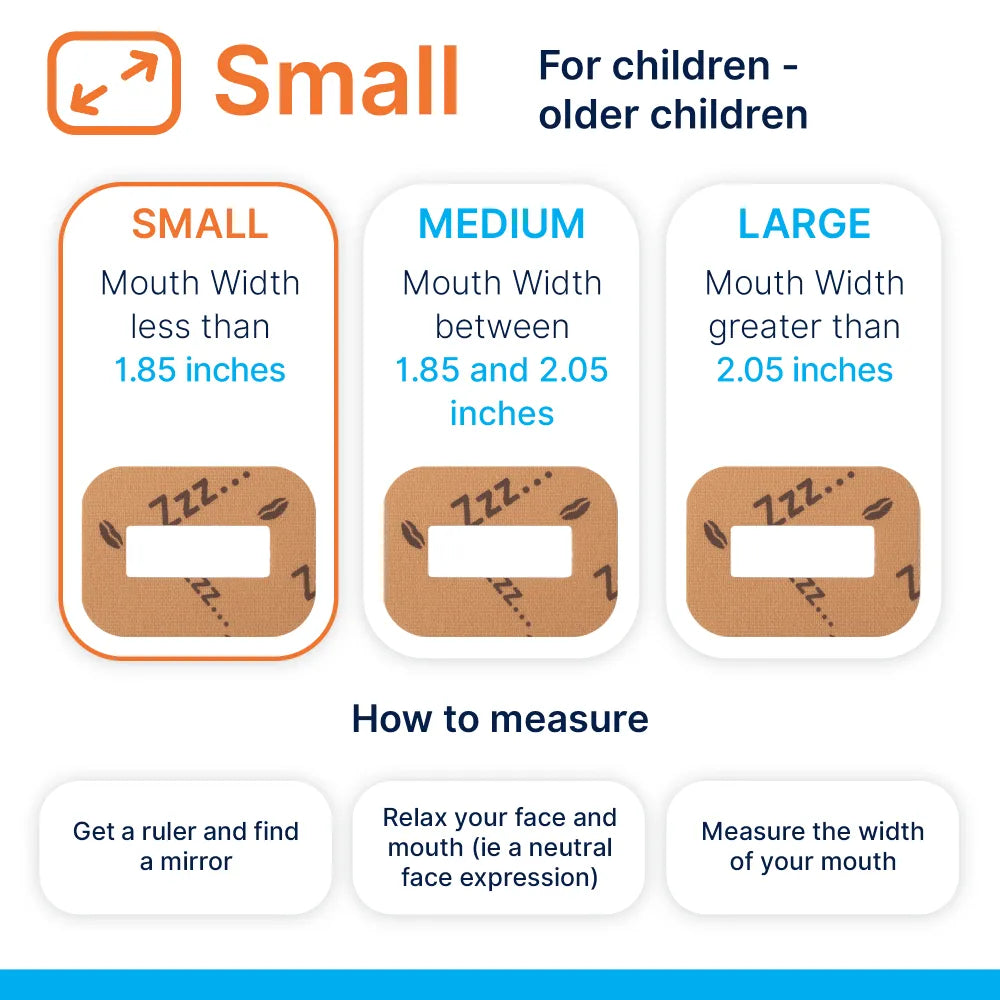
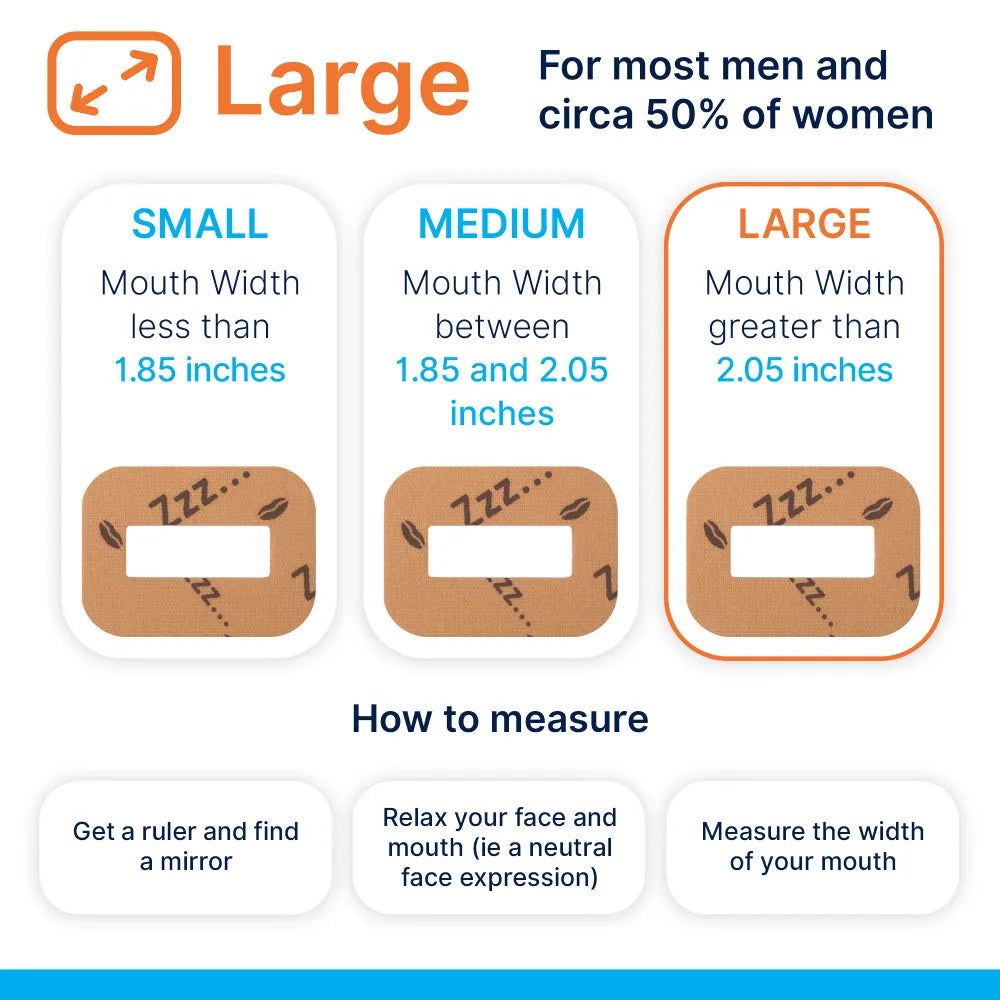
There are sizes designed for small faces and for older children. The adhesives used are similar to medical tapes and usually latex free. Even so, a patch test is wise before regular use.
It is not a cure on its own. It is a tool that can reinforce better breathing while the real causes of mouth breathing are assessed and treated.
Who might benefit
Children who can breathe through the nose once reminded, but tend to forget and slip back to an open-mouth rest, are the most likely candidates. These are often the children who can close their mouth easily for a photo, then relax back to parted lips a moment later.
If a child has had enlarged tonsils, allergies or frequent colds, a habit can persist even after the nose is clear. A gentle prompt helps the new habit stick.
Age matters. Many families start around school age. Very young children cannot reliably remove tape on their own and may not understand the purpose. As a rough guide, daytime practice from about 4 years can work in some cases, moving only to supervised sleep use when a child shows they can manage it comfortably for extended periods and can remove the tape quickly by themselves.
If in doubt, ask a paediatric dentist, ENT doctor or an orofacial myologist for guidance.
Safety first
There are times when lip taping is not appropriate. Park the idea and seek assessment if any of the following apply:
- Recurrent or loud snoring
- Observed pauses in breathing, gasping, or laboured breathing during sleep
- Frequent night sweats, bedwetting beyond the usual age, severe daytime sleepiness or behaviour suggesting poor sleep
- Blocked nose from a cold, flu or hay fever flare-up
- Known nasal obstruction, significant deviated septum, nasal polyps or chronic sinus issues
- Uncontrolled asthma, chronic cough or frequent wheeze
- Gastro-oesophageal reflux with regurgitation, or a tendency to vomit at night
- A seizure disorder
- Craniofacial syndromes or neuromuscular conditions affecting airway control
- Skin conditions around the mouth, severe eczema or adhesive allergy
General safety rules help too:
- The child must be able to remove the tape without help and should practise doing so.
- Start with short, fully supervised sessions while awake.
- Do not use during illness or if the nose feels stuffy.
- Night-time use is only considered after easy daytime sessions and with a clinician’s input if there are any red flags.
A step-by-step way to start
A calm, staged approach makes this simple and child friendly.
- Check the nose
- Ask the child to close their lips and breathe lightly through the nose for a minute. If they struggle, address the nose first.
- Try a gentle saline spray once or twice a day during seasonal allergy periods.
- Ask your GP or pharmacist about allergy care if sneezing and congestion are frequent.
- Build lip awareness
- Dot a tiny bit of lip balm at the centre of the upper and lower lips and ask the child to “kiss the dots” together for a few breaths.
- Practice holding a paper straw or a button between the lips for 10 seconds, rest, repeat 3 to 5 times.
- Turn it into a game with a sand timer.
- Patch test the tape
- Apply a small piece to the cheek for 15 minutes. Check the skin later for redness or irritation.
- First sessions
- Place the tape around the mouth while reading together or watching a short cartoon.
- Start with 10 minutes, then 15 to 20 minutes. Keep it light and positive.
- Agree a signal so the child can ask for a break without fuss.
- Build time
- Once 20 minutes feels normal, move to 30 to 60 minutes during calm activities.
- Aim for two short sessions daily rather than a single long one early on.
- Consider sleep only when ready
- If daytime sessions are easy for a couple of weeks, consider a supervised nap.
- Use a baby monitor or sit nearby for the first few trials.
- If there is any noisy breathing or restlessness, remove the tape and pause the plan while you seek advice.
Daytime practice and night-time use
Daytime is where habit change is made. The child is alert, you can supervise closely and feedback is immediate. Over time the lips learn to stay closed without the tape, especially during screen time, homework or car rides where posture tends to sag.
Night-time is a separate conversation. The body behaves differently during sleep and snoring can appear only at night. If you have any doubts about sleep quality, get a professional opinion first. When your clinician is happy and daytime use is comfortable, brief and supervised naps are a reasonable next step.
The goal is not to use tape forever. It is to build the skill and strength for a natural seal that holds on its own.
Root causes to address alongside taping
A successful plan looks beyond the tape.
-
Nasal health
Treat allergies, reduce irritants at home and use saline rinses in pollen seasons. A cool-mist humidifier can help in dry rooms. -
Muscle tone and tongue posture
An orofacial myologist or myofunctional therapist can set exercises that bring the tongue to the palate, strengthen the lips and improve swallowing patterns. -
ENT assessment
Enlarged adenoids or tonsils, chronic congestion or structural blockage can keep the mouth open. If present, tape will not fix the problem on its own. -
Dental and orthodontic support
A narrow palate and dental crowding are often linked with mouth breathing. Palatal expansion or other appliances may be advised by a paediatric dentist or orthodontist. Good breathing habits make these treatments more effective. -
Habits at home
Encourage chewing of real food textures, regular outdoor play that involves nasal breathing, upright posture and a consistent bedtime. Screens tend to invite slack posture and open mouths, so set reminders during screen time to bring lips together.
What the research tells us
High quality trials in children on lip taping itself are scarce, which is typical for newer habit tools. What we do have are several strands of evidence that point in the same direction.
- Nasal breathing supports airway conditioning and appears to reduce upper airway resistance compared with oral breathing.
- Myofunctional therapy in children with sleep disordered breathing shows improvements in symptoms and sometimes in measured airway indices.
- Small studies in adults using mouth taping report reduced snoring and mouth breathing, along with better perceived sleep quality.
- Dental research has long linked mouth breathing with dry mouth, caries and gingival inflammation.
This suggests taping can be a useful prompt for some children when combined with proper assessment and care. It should not be used to mask signs of sleep apnoea or to ignore ongoing nasal blockage.
Common questions from parents
-
Will my child be able to breathe?
The child versions sit around the mouth and do not seal the lips shut. A child can part the lips if needed and should always be able to remove the tape. -
How long before it makes a difference?
Some children improve lip seal during the day in a couple of weeks. Night-time habits can take longer. Growth and orthodontic change take months to years, so patience matters. -
Can this change facial growth?
Function influences growth, especially while the face is developing. Supporting healthy posture helps the direction of growth, but it is not a replacement for orthodontic care when structural change is needed. -
Will it stop drooling?
Better lip tone and nasal breathing often reduce drooling. If it persists, ask your dentist or paediatrician to check for other causes. -
Is school use a good idea?
Home use is easier to manage and avoids attention from peers. Some families use it during homework or reading time rather than at school. -
What if my child dislikes the feeling?
Go slower. Use smaller pieces, try a different fabric or model the habit yourself. Pair it with a reward chart so it stays positive.
Practical tips for comfort and consistency
- Clean and dry the skin around the mouth before application.
- Warm the tape between your fingers to soften the adhesive.
- Apply from the centre outward so it sits evenly.
- Use a thin barrier cream on the outer lip line if skin is sensitive, keeping it away from the adhesive area to prevent slipping.
- Replace the tape each session. Reusing weakens adhesion and can irritate the skin.
- Give it a friendly name, like “breathing band,” and let your child choose the colour if options exist.
- Keep tissues and a nasal spray handy in case the nose needs a quick clear.
- Track progress with a simple chart. Small wins build momentum.
A quick reference table
| Situation | What to do | Notes |
|---|---|---|
| Child under 4 years | Hold off on taping | Focus on nasal care, lip games and gentle reminders |
| Stuffy nose or current cold | Do not use | Resume only when nasal breathing is easy at rest |
| Mild open-mouth habit while awake | Daytime sessions 10 to 20 minutes, build slowly | Pair with myofunctional exercises |
| Light snoring without other concerns | Speak to GP, dentist or ENT first | Consider a trial only with professional reassurance |
| Ongoing orthodontic treatment | Coordinate with the orthodontist | Better lip seal can support appliance outcomes |
| Skin sensitivity or eczema | Patch test, barrier cream, shorter sessions | Stop if redness or itching persists |
| Observed pauses in breathing at night | Avoid taping | Seek sleep clinic or ENT assessment promptly |
A sample two-week starter plan
Week 1
- Day 1 to 3: Lip awareness games twice daily, 5 minutes each. Patch test tape on cheek.
- Day 4 to 7: Apply tape for 10 to 15 minutes during quiet reading, once daily. Note comfort and nasal ease.
Week 2
- Day 8 to 10: Increase to 20 to 30 minutes, once or twice daily.
- Day 11 to 14: Maintain 30 to 45 minutes. If all is comfortable and there are no sleep concerns, discuss next steps with your clinician before trying a supervised nap.
Keep the plan flexible. If a day feels off, shorten the session or skip it.
When to seek professional guidance
- Snoring that persists or worsens
- Pauses in breathing, gasping or choking sounds at night
- Frequent bedwetting after the usual age, morning headaches or marked daytime behaviour issues
- Mouth breathing that continues despite good daytime practice
- Repeated ear infections, chronic nasal symptoms or suspected enlarged adenoids and tonsils
- Dental crowding, crossbite or concerns about jaw growth
- Any worry that the child dislikes or struggles with the tape
A paediatric dentist, ENT specialist, GP, speech and language therapist with orofacial focus, or an orofacial myologist can help. Taping is one tool. The real progress comes from matching the tool to the child, treating causes and building habits that last.


















0 comments