Breathing through the nose while asleep sounds simple, yet for many people it is rare. Mouth breathing links to snoring, dry mouth, fragmented sleep, and in some cases obstructive sleep apnoea. That is why tapes that encourage lip seal have gained attention. Among them, MyoTape is often discussed by clinicians in sleep clinics and dental practices. The big question is not whether the idea is appealing, but what the evidence actually says.
Below you will find a clear survey of what has been studied, what remains uncertain, and how health professionals are using perioral taping in practice. The focus is on clinical data related to MyoTape and near neighbours in the same category.
What MyoTape is, and how it differs from generic mouth tape
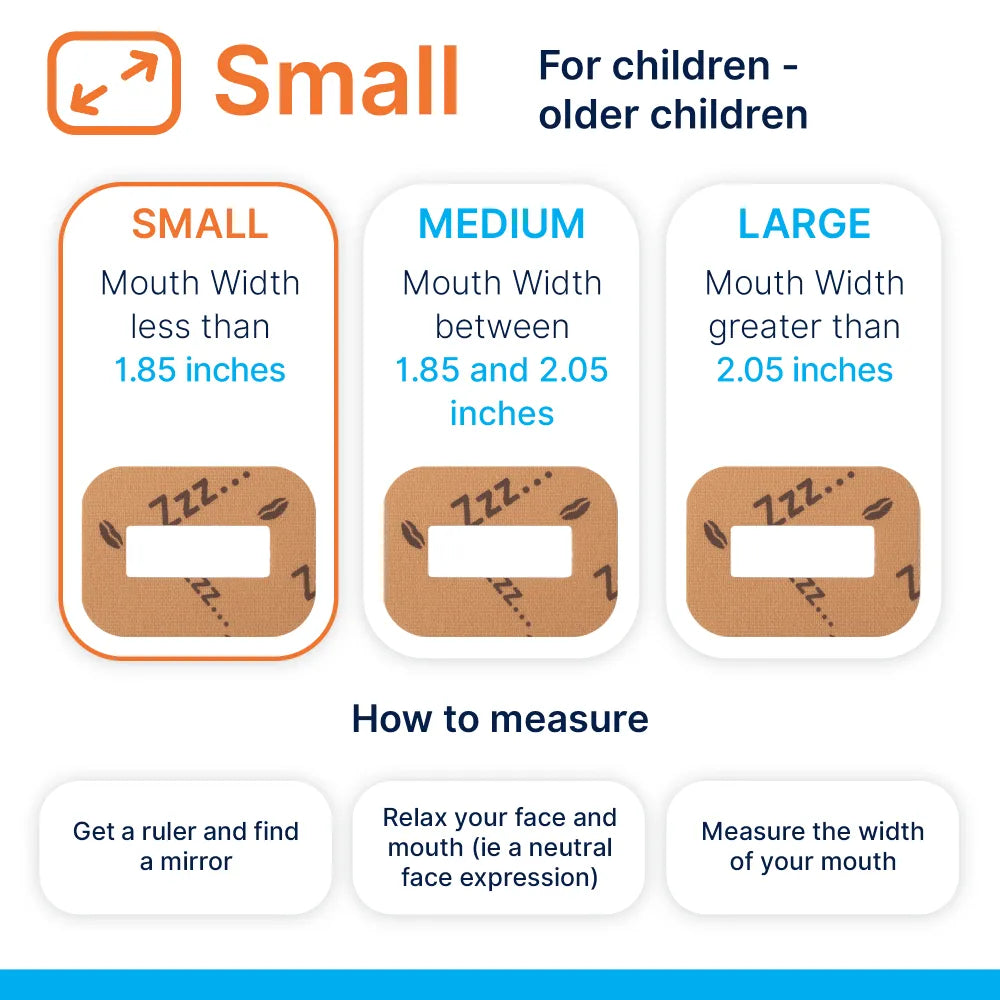
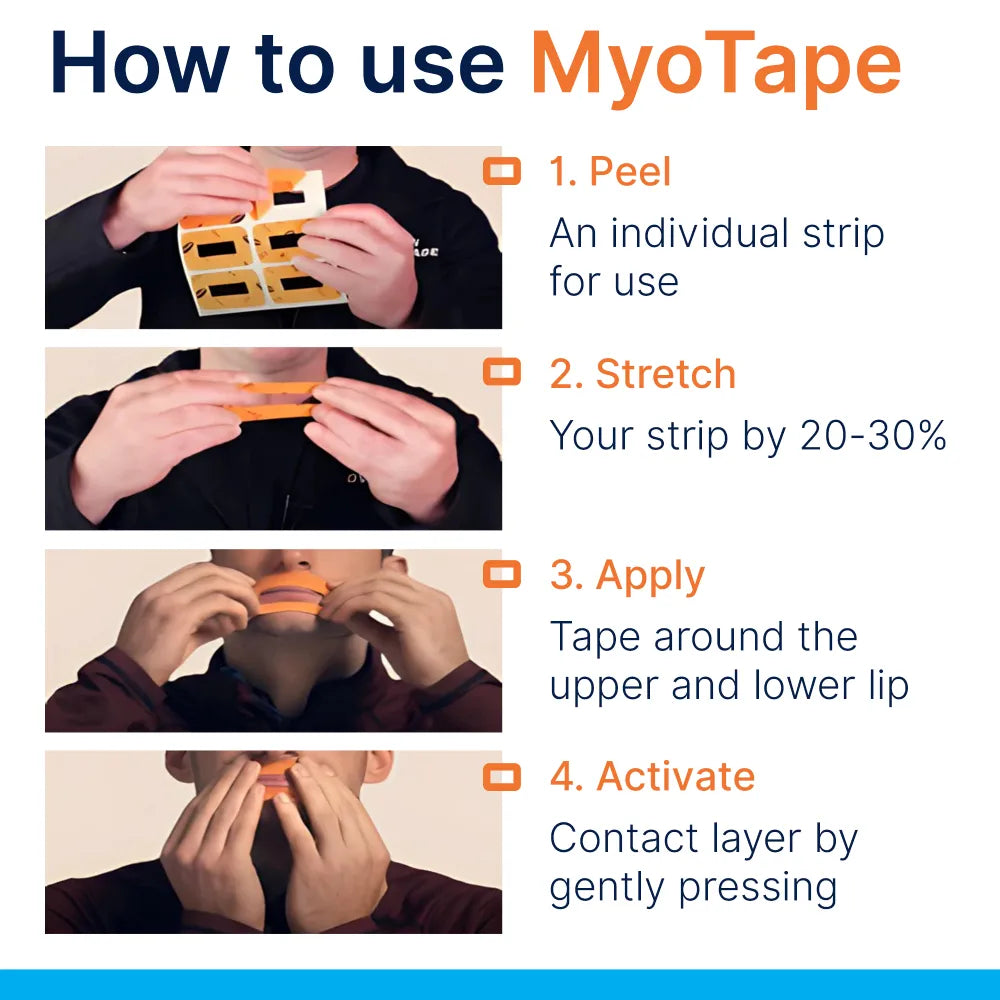
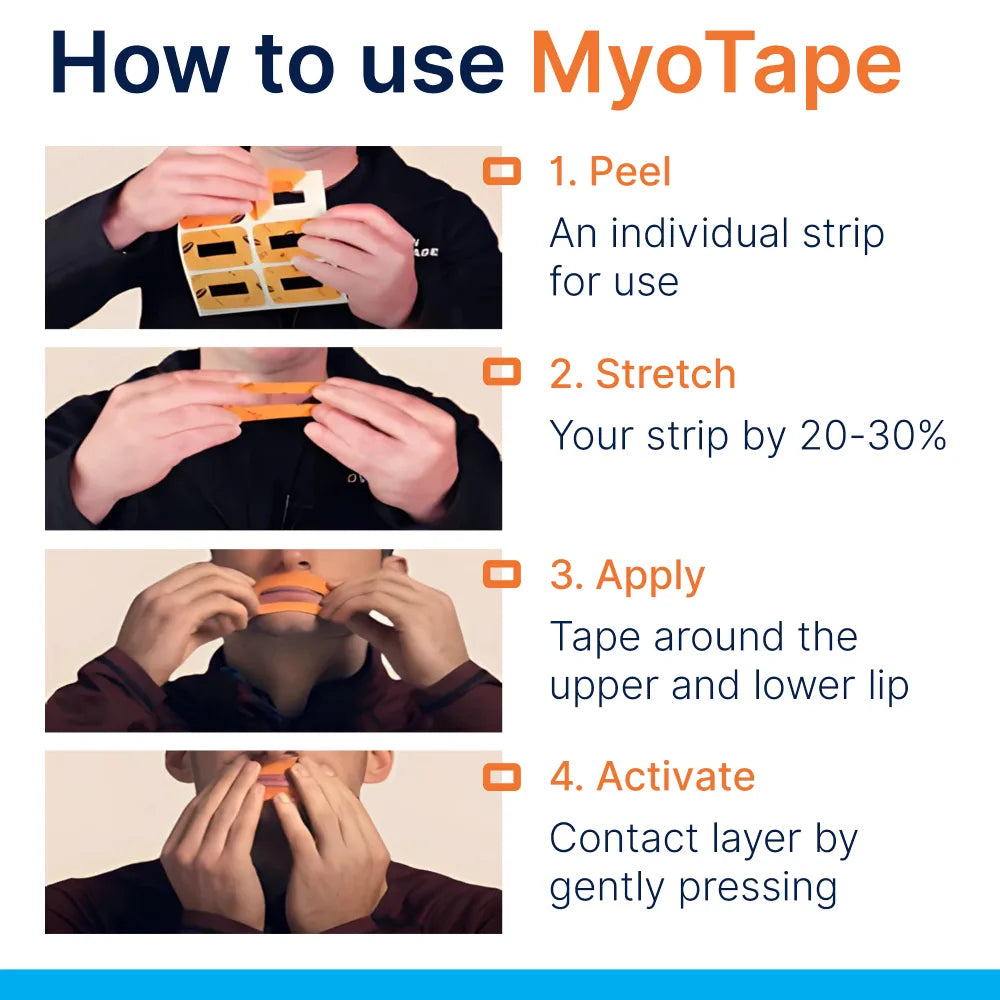
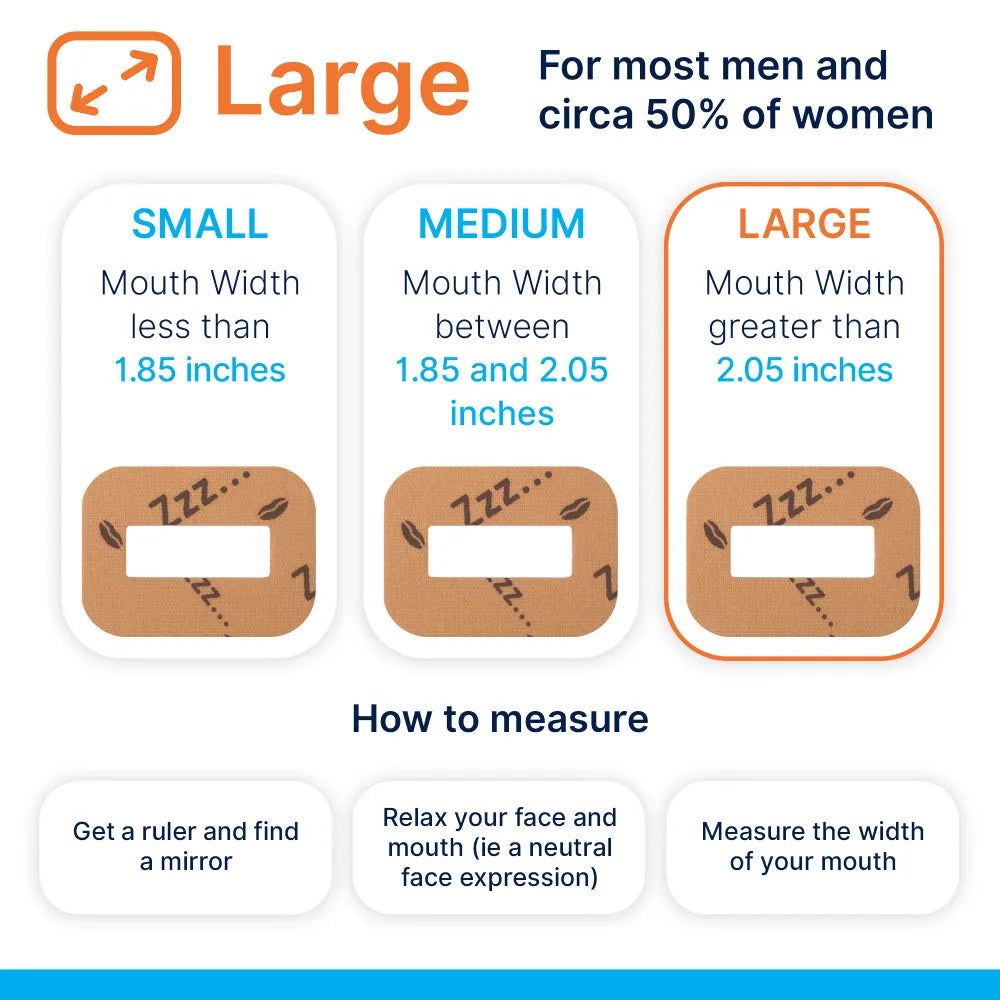
Most mouth tapes close the lips by placing adhesive directly across them. MyoTape takes a different route. It is an elastic, perioral strip that sits around the lips and gently draws them together while leaving a small central opening. The intent is to nudge nasal breathing, not to seal the oral cavity air-tight.
This design matters for two reasons:
- It lowers the risk of panic for first-time users who worry about a fully sealed mouth.
- It can be paired with myofunctional therapy, since it supports lip seal while the tongue adopts a more elevated posture.
The product shows up both in adult sleep clinics and paediatric airway programmes. Many clinicians view it as a behavioural prompt that blends into a wider care plan rather than a stand-alone fix.
Where the research stands right now
Clinical trials that name MyoTape specifically remain limited in number and size. The broader literature on lip taping, nasal breathing aids, and orofacial myofunctional therapy is larger, though still early-stage by typical medical standards.
In summary:
- Adult studies on lip taping tend to focus on snoring and mild obstructive sleep apnoea with mouth breathing. Several small trials and crossover studies show reductions in snoring time and subjective sleepiness, and modest drops in apnoea-hypopnoea indices in select groups.
- Paediatric work often sits within orthodontic or orofacial therapy programmes targeting lip incompetence, open mouth posture, and sleep-disordered breathing symptoms. Here, tapes that support lip seal, including perioral designs, appear as adjuncts alongside breathing exercises and habit change.
- Safety reporting is encouraging in carefully selected patients with adequate nasal patency. Skin irritation, anxiety on first use, and poor tolerance are the most frequent issues described.
Robust head-to-head trials comparing specific brands, including MyoTape, are not yet common in peer-reviewed journals. Most clinical claims sit on a mix of pilot trials, service evaluations, and practitioner reports.
The big questions that clinical studies try to answer
Researchers and clinicians tend to circle around four practical questions.
- Does perioral taping reduce snoring in habitual mouth breathers at night?
- Can lip seal prompt better sleep quality and next-day alertness in mild conditions?
- Is it safe for the right patients, and what screening keeps risk low?
- For children, does supporting lip seal assist myofunctional goals and dental arch growth when combined with other therapy?
The answers are trending positive in narrow groups, although the certainty level is still modest.
Snapshot of the current evidence
| Evidence area | Population | Intervention | Outcomes reported | MyoTape named | Confidence level |
|---|---|---|---|---|---|
| Adult snoring | Primary snorers with mouth breathing | Lip taping or perioral tape at night | Reduction in snoring duration and intensity on home recordings; improved bed-partner reports | Sometimes unspecified; brand often not stated | Moderate for symptom change in selected users |
| Mild OSA | Mild OSA with open-mouth pattern | Lip taping at night, sometimes with nasal dilators | Small improvements in AHI and oxygen desaturations in subsets; better subjective sleep quality | Brand variably reported | Low to moderate due to small samples |
| CPAP tolerance | Adults on CPAP with mouth leak | Perioral taping in addition to CPAP | Lower leak and improved comfort in some clinic reports | Occasionally | Low due to observational nature |
| Paediatric airway and orthodontics | Children with mouth breathing and lip incompetence | Perioral tape during training sessions and sleep; paired with myofunctional therapy | Improved lip seal habit, better tongue posture adherence, lower daytime mouth breathing by caregiver report | Frequently mentioned by programme protocols | Low to moderate for habit change |
| Safety | Mixed adult and paediatric | Perioral tape use under screening | Mostly minor skin irritation; anxiety on first use; discontinuation if nasal patency poor | Yes | Moderate for near-term safety in screened users |
Confidence levels above reflect the quality and volume of published data rather than clinician enthusiasm. Small trials are promising, yet many rely on short follow-up and device-agnostic methods.
What the more rigorous studies tend to show
A few patterns recur across better designed investigations.
- Primary snorers who mouth breathe at night often respond best. Night-time recordings show a fall in snoring minutes and sound intensity in this group.
- Mild OSA patients with adequate nasal airflow see modest gains. Drops in apnoea-hypopnoea indices appear in some studies, although not in all participants.
- Adding a nasal dilator or saline rinse boosts tolerance and benefit for those with borderline congestion.
- Daytime myofunctional exercises plus perioral taping support carryover to sleep. Programmes report stronger adherence to tongue posture and lip seal when both are used.
Importantly, moderate to severe OSA usually requires more than a tape. Clinicians stress that airway collapse in those cases demands proven treatments like CPAP, oral appliances, positional therapy, or surgery. Tape can still help with mouth leak on CPAP, but it is rarely the main therapy.
Why encouraging nasal breathing might help
Nasal airflow is not just air through a different route. It offers physiological advantages that matter during sleep.
- Filtration and humidification reduce dryness and sore throat.
- Nasal nitric oxide is higher, which influences ventilation and may aid gas exchange.
- Lip seal supports tongue-to-palate posture, which can increase retropalatal space in people with low tongue tone.
When mouth breathing is habitual, tissues dry out and the tongue sits low. Gentle elastic support around the lips can remind the system to choose the nose by default.
Safety first: who should not use perioral tape
No tape is right for everyone. Simple screening avoids problems.
Avoid use in:
- Moderate to severe OSA unless managed by a sleep team
- Significant nasal blockage or chronic sinus disease
- Recent nasal or oral surgery
- Active vomiting risk, reflux with nocturnal regurgitation, or severe nausea
- Severe cardiopulmonary disease without medical oversight
- Panic disorder, claustrophobia, or high anxiety around airway sensations
- Skin conditions or allergy to adhesives
- Children without direct guidance from a clinician experienced in paediatric airway care
Even in low-risk groups, start with short, supervised trials while awake, then step up to sleep once comfort is clear.
How clinicians are applying MyoTape in practice
Across clinics, MyoTape tends to play one of three roles.
-
As a prompt for nasal breathing in primary snorers
Adults with clear nasal airflow and clear mouth breathing signs at night receive MyoTape along with nasal hygiene advice. They use a snoring app or bed-partner reports to monitor change. -
As part of CPAP care for mouth leak
Users with good mask fit but high leak may try perioral tape after a mask refit and humidification tweaks. Reduced leak can raise effective pressure delivery and comfort. -
Within paediatric airway and orthodontic programmes
Children practise lip seal during daytime tasks and short reading sessions, then progress to night use once comfortable. The tape supports training goals set by myofunctional therapists and airway-aware dentists.
In each scenario, the tape is a nudge, not the whole plan. Breathing exercises, nasal care, positional coaching, weight management, and dental or ENT input round out the approach.
A practical clinic protocol that keeps things safe
A simple pathway helps teams standardise care.
-
Screen
- STOP-Bang or equivalent for OSA risk
- Nasal airflow check with Cottle manoeuvre or rhinomanometry if available
- Skin sensitivity and anxiety check
-
Prepare
- Saline rinse, steroid spray if prescribed, and gentle nasal warm-up
- Patch test the adhesive on the cheek for 24 hours
-
First exposure
- Place the tape while awake for 5 to 10 minutes during quiet reading
- Teach finger release at the central gap if anxious
- Progress to a daytime nap, then to night use
-
Combine
- Add nasal dilator strips for borderline nasal patency
- Pair with orofacial exercises to reinforce tongue posture
- Adjust bedtime position and reduce alcohol on trial nights
-
Measure
- Use a snoring app or bed-partner ratings over two weeks
- Track Epworth Sleepiness Scale or a clinic-approved sleepiness tool
- For OSA, use home sleep testing when indicated to check AHI effects
-
Review
- If no gain after two weeks, stop or revise the plan
- If irritation or anxiety appears, pause and reassess fit, skin prep, or suitability
What counts as a good response
Clinicians usually look for one or more of the following:
- A clear drop in snoring minutes and peak volume on app data
- A better bed-partner report on nightly quietness
- Improved mouth moisture and less morning hoarseness
- Lower next-day sleepiness in those with mild symptoms
- Reduced CPAP leak if that was the target
If none of these shift, the person may need a different tactic.
What to tell patients who ask direct questions
Simple, honest messages help people use the tape correctly.
- It aims to nudge nasal breathing, not to shut the mouth completely.
- It works best when the nose is clear. Treat congestion first.
- It is not a cure for moderate to severe apnoea.
- You can remove it with one finger at the central gap at any time.
- It should feel gentle, not tight. If it pulls painfully, the fit or product size is off.
- Results appear over days to weeks. Keep notes so the clinic can judge progress.
What the paediatric angle looks like
Children with open mouth posture often show lip incompetence, low tongue tone, and a high, narrow palate. Perioral tape has become a common adjunct in airway-aware dental and therapy programmes because it supports the habit change required for stable results.
Key points that teams emphasise:
- Screening for adenotonsillar hypertrophy and nasal blockage comes first.
- Perioral tape is used alongside exercises that raise tongue posture and strengthen the lips.
- Parents supervise early sessions. Many start with TV time or book reading to build comfort.
- Night-time use waits until the child shows easy tolerance while awake.
Reports from clinics point to better daytime lip seal and fewer dry mouth complaints. Formal trials with longer follow-up will help judge effects on arch development and sleep metrics.
What remains to be tested
Several research gaps are ready for well-structured trials.
-
MyoTape-specific randomised trials with adequate power
Study designs could compare MyoTape with sham taping or with standard care in primary snorers and mild OSA mouth breathers, using home sleep testing and validated questionnaires. -
Paediatric outcomes with objective measures
Trials that track lip seal habit, tongue posture, sleep quality, and arch changes over 6 to 12 months would be valuable. -
CPAP users with mouth leak
Controlled studies on leak rates, adherence, comfort, and residual AHI could guide policy in sleep clinics. -
Safety over months rather than weeks
Longer follow-up on skin, tolerance, and adherence would build confidence for routine use. -
Predictors of response
Clear criteria based on nasal resistance, craniofacial features, and behavioural factors would help select the right patients.
Tips that improve tolerability from day one
Small steps can make a big difference.
- Clean, dry skin before application
- A gentle moisturiser applied in the morning, not at night
- Trimming facial hair where the tape sits
- Warming the tape between fingers before placement to increase flexibility
- Slight smile while applying to find a neutral tension
- Keeping the central opening visible to reassure first-time users
Most people who abandon taping do so after the first night. With better coaching and gradual exposure, acceptance rises.
How to read claims you see online
Marketing language often runs ahead of evidence. A careful reader looks for:
- Peer-reviewed trials with clear methods and objective outcomes
- Details on who was studied, since selection matters a lot
- Long enough follow-up to judge real-world effect
- Brand-specific data rather than device-agnostic claims if the promise hinges on a design detail
- Safety reporting that includes dropouts and adverse events, not just success stories
Curiosity is good. So is healthy scepticism.
What a realistic care pathway can look like
For a typical adult with loud nightly snoring, dry mouth on waking, and clear nasal airflow:
- Week 1: Nasal hygiene routine, trial of perioral tape while awake, then short naps
- Week 2: Night-time use on four nights, snoring app running, alcohol cut-back
- Week 3: Review in clinic, results discussed; continue if benefits clear
- Month 2: If snoring persists, consider nasal dilator, myofunctional training, or oral appliance referral
- Ongoing: Periodic breaks to check if habit change persists without the tape
For a child with mouth breathing and open mouth posture:
- ENT and dental screening to rule out airway obstruction
- Parent education, playful daytime practice with perioral tape
- Integration with tongue posture drills and chewing tasks
- Night-time use when ready, with check-ins every 4 to 6 weeks
- Reassess growth, sleep, and symptoms at 6 months
The take-home for clinicians
- Evidence for perioral taping is promising for primary snoring and mild OSA in mouth breathers with clear nasal airflow.
- MyoTape’s design suits programmes that target habit change and tongue posture, thanks to its perioral approach with a central opening.
- Safety and success depend on screening, gradual exposure, and combined care plans.
- High-quality, brand-specific trials will clarify where the product fits best in routine practice.
Until those papers arrive, careful patient selection, honest messaging, and simple measurement tools can deliver meaningful gains for many people who want quieter nights and a more rested morning.


















0 comments