Breathing through the mouth dries the mouth, changes saliva chemistry, and nudges the oral microbiome in an unfriendly direction. Over months and years that can feed into cavities, inflamed gums, and even jaw growth patterns in children that make crowded teeth more likely.
A simple elastic tape that encourages lips to stay together during rest and sleep can interrupt that cycle. That is where myofunctional taping products step in, with a design that sits around the lips and reminds them to meet without blocking the central opening. Many people know this category by a brand name, and dentists are now seeing it as a practical adjunct to daily hygiene and diet.
Why nasal breathing matters for teeth and gums
Nasal breathing supports oral health in several ways.
- Saliva protects enamel. It buffers acids after meals and brings minerals that remineralise early white spot lesions. Mouth breathing reduces saliva flow and dries the lips, cheeks, and tongue, which raises acidity and supports acidogenic bacteria.
- The nose filters and conditions air. Air that arrives through the nasal passages reaches the back of the mouth and throat at a friendlier temperature and humidity, and with nitric oxide from the sinuses that influences vascular tone and antimicrobial defences.
- Lips together with the tongue resting on the palate support stable dental arches. This resting posture helps keep the maxilla broad and the bite balanced, particularly during growth.
When lips hang open at rest, the balance above shifts. Plaque matures faster, breath smells worse in the morning, and gums can look shiny and inflamed along the margins.
Mouth taping, but not as you think
People often picture a strip across the lips. That is not necessary for many, and it can feel alarming to newcomers.
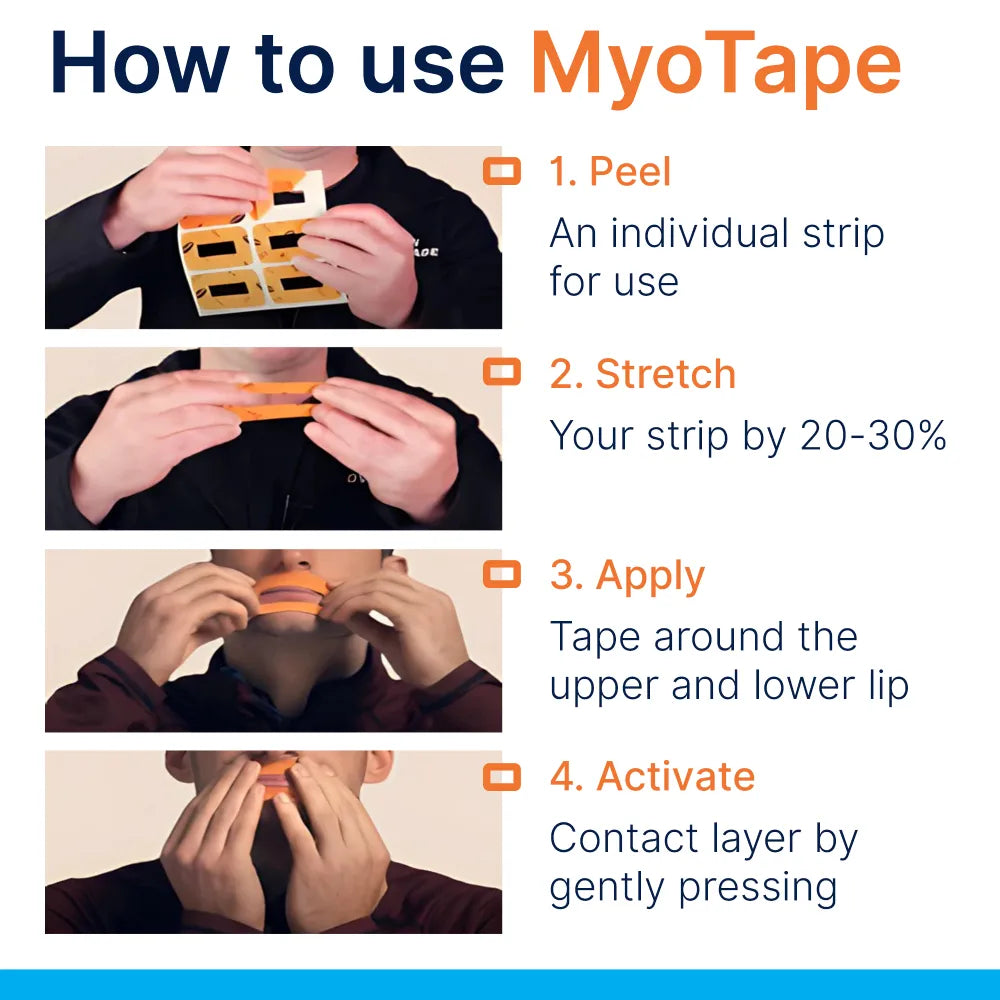
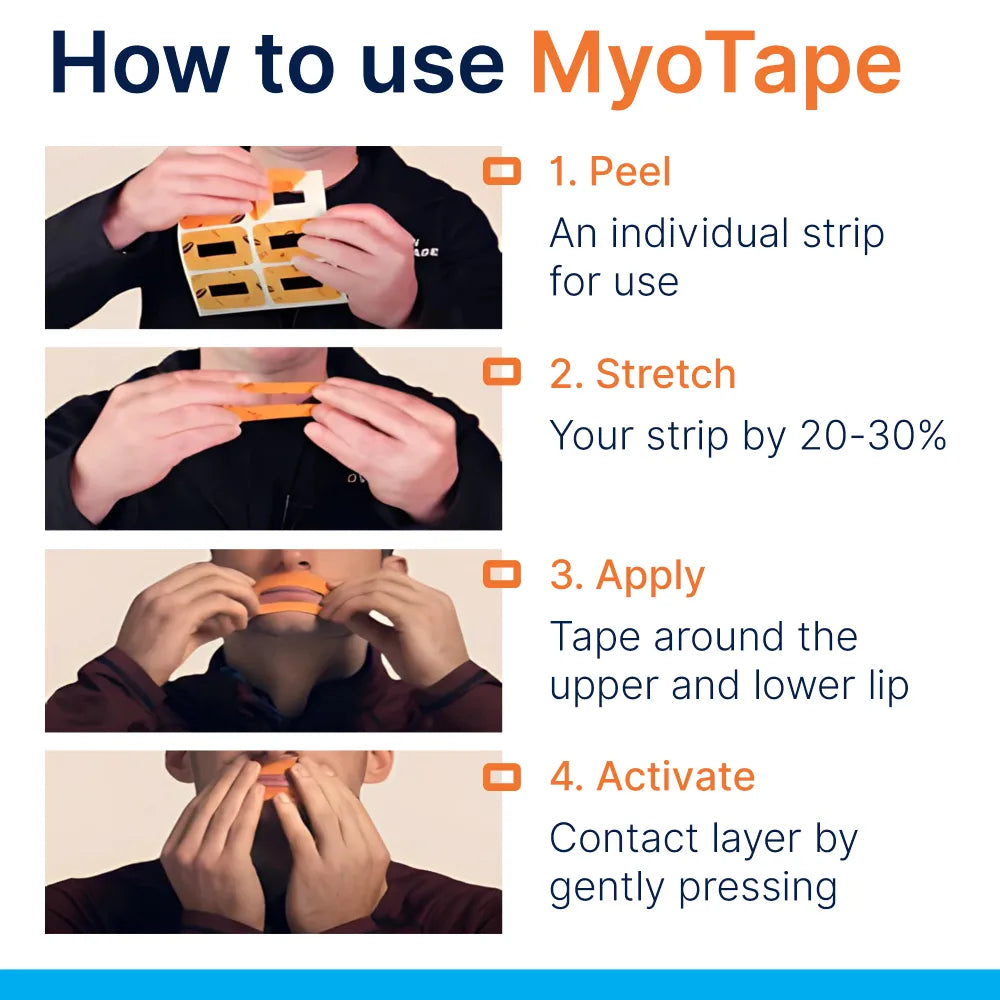
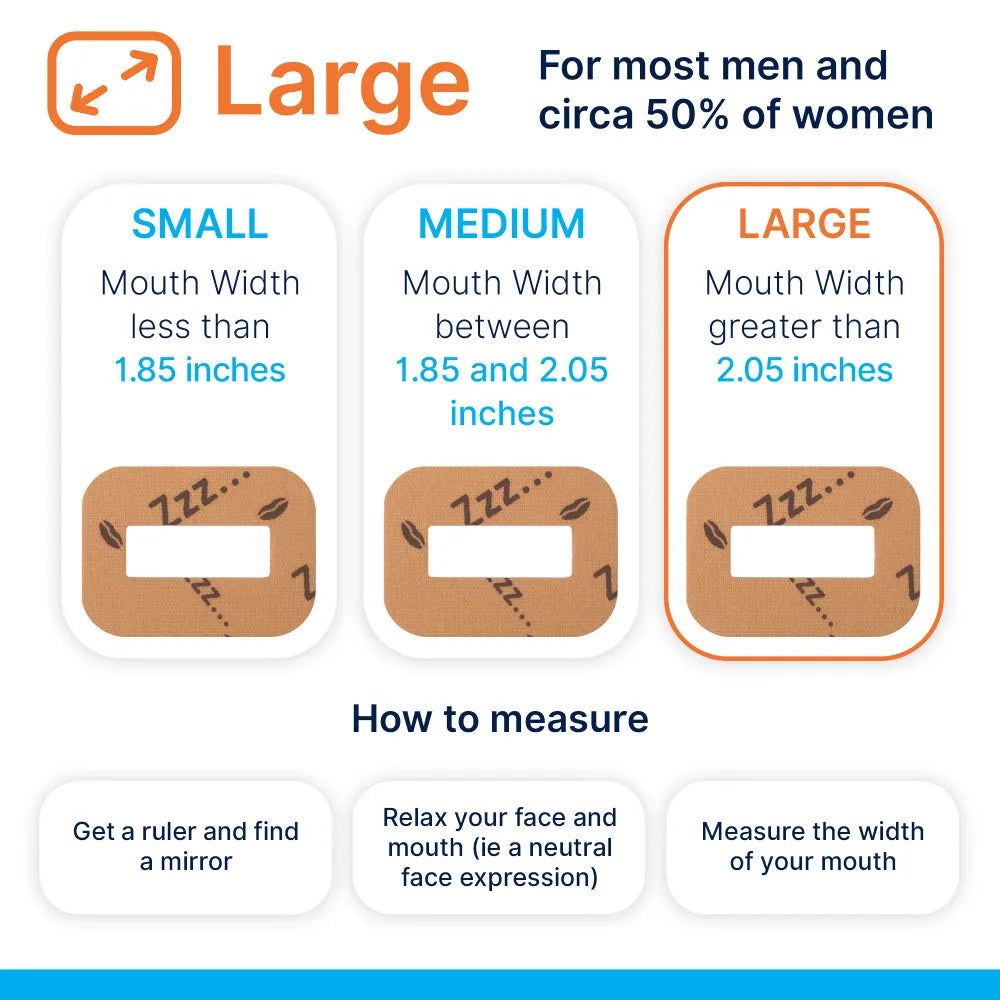
An around-the-mouth tape uses a soft elastic ring with a central opening. It sits on the skin around the lips and gently encourages the lips to meet. You can still part the lips if you need to cough or speak. If the nose blocks during the night, you can open the mouth without tearing anything off in a panic.
The aim is a prompt for lip seal, not force.
What the research indicates
The link between mouth breathing and dental disease is established. Dry mouth is tied to higher rates of decay and periodontitis, and even short periods of open-mouth exposure lower plaque pH and slow the return to neutral after sugar.
The evidence base for taping itself is growing. Small studies and clinical reports show that taping can reduce snoring intensity and mouth breathing during sleep in selected adults. Direct trials on dental outcomes are limited, though the mechanisms are well mapped: more saliva on the teeth at night, less evaporation, a friendlier pH profile, and a shift in oral microbial balance away from species that thrive in dry, acidic niches.
Clinicians also report better tolerance of myofunctional exercises when lip seal is supported at night, and parents often notice less drooling on pillows in children who switch to nasal breathing.
Dental problems linked with open-mouth breathing
Patterns vary by person, but the common threads are familiar to any dental team:
- Cavities, especially along cervical margins and interproximally
- Gingivitis with bleeding on brushing and flossing
- Periodontitis risk rising with chronic dryness and plaque retention
- Halitosis on waking, sometimes persisting through the day
- Enamel erosion from frequent acidic episodes and low buffering capacity
- Orthodontic crowding and long-face growth patterns in children
- Mouth ulcers and angular cheilitis that keep recurring
- Tartar build-up that accelerates between hygiene visits
These are not always caused by mouth breathing alone, yet lip seal is an easy variable to test and often a missing piece of the puzzle.
How an elastic lip tape supports routine dental care
Think of it as a small tool that multiplies the effect of habits you already recommend:
- Toothbrushing with fluoride toothpaste morning and night
- Daily interdental cleaning with floss or brushes
- Smart snacking patterns and mindful sugar frequency
- Saliva-friendly choices, for example sugar-free gum after meals
- Regular maintenance with a hygienist
By protecting the moisture environment at night, the tape helps all of the above work better. Patients often report that their mouth feels less dry on waking and that brushing is more comfortable.
Getting started safely
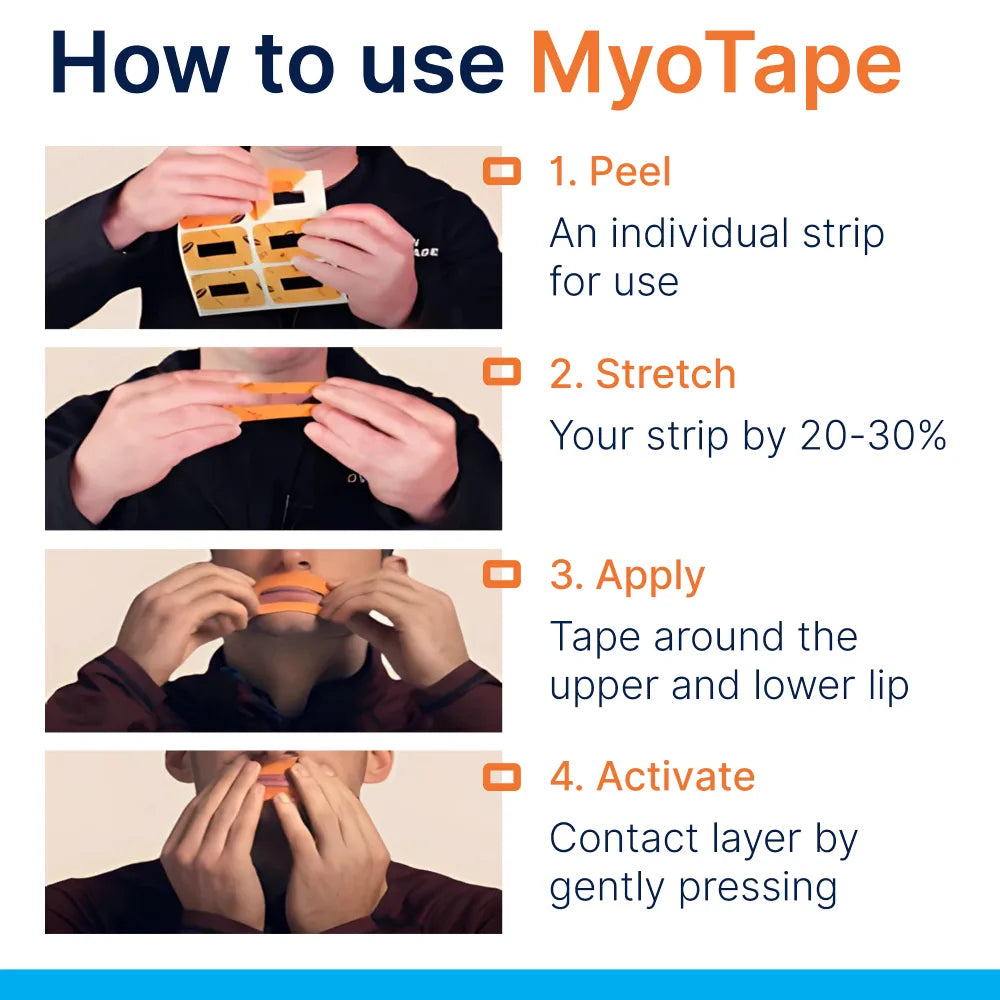
A short, careful set-up helps people accept the idea and stick with it.
- Patch test the adhesive on a small spot near the corner of the mouth for 15 minutes during the day. Check for redness or irritation.
- Prepare the skin. Cleanse gently, dry completely, and avoid heavy moisturisers where the tape will sit, as they can weaken adhesion.
- Trim facial hair where possible. Beards or heavy stubble reduce adhesion and can tug on removal. If trimming is not an option, position the tape slightly higher on the skin that is hair-free.
- Start while awake. Apply the tape, rest with lips together, and breathe through the nose for 10 to 15 minutes. This builds confidence.
- First nights, set a short trial. Use the tape for the first half of the night or during a nap. Keep a glass of water and tissues nearby, and remove if you feel any distress.
- Removing the tape, warm it with your fingers, stretch the elastic gently to reduce pull, and peel slowly. A drop of warm water or a thin layer of water-based moisturiser can make removal kinder.
Consistency matters more than perfection. Even a few nights a week often leads to noticeable changes.
Who should not use it, and when to seek advice
Avoid lip taping if any of the following apply until you have professional guidance:
- Severe nasal obstruction or airflow limitation
- Untreated obstructive sleep apnoea or frequent pauses in breathing during sleep
- A current respiratory infection with significant congestion
- Recent vomiting, nausea, or a condition that raises aspiration risk
- Heavy alcohol intake or sedative use before bed
- Skin conditions around the mouth that flare with adhesives, for example eczema or contact dermatitis
- Latex or adhesive allergies unless you know the product is free of the trigger
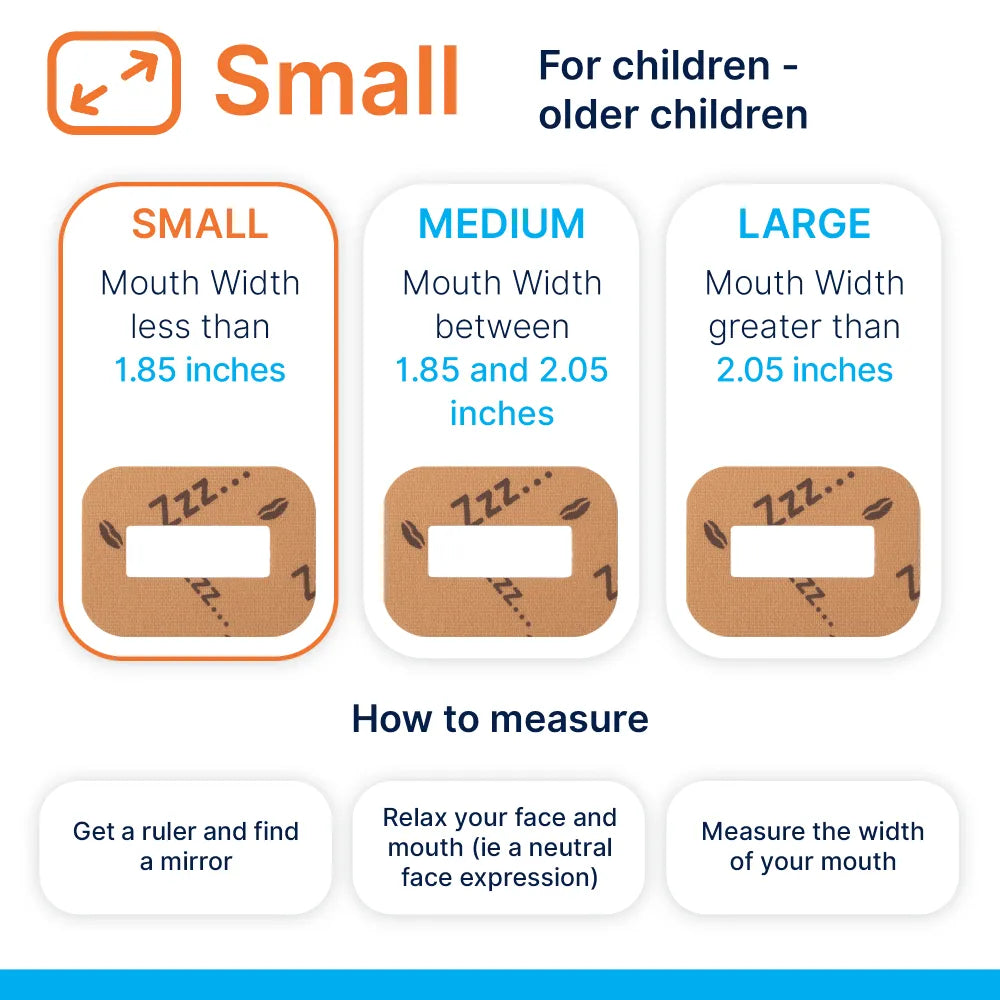
Children need close supervision, with an adult present when the tape is in use and an age-appropriate size that never blocks the mouth. If a child snores most nights, breathes through the mouth in the day, or has recurrent ear or sinus infections, seek assessment with a dentist and possibly an ENT specialist. Tapings are not a substitute for medical care.
Supporting nasal breathing through the day
Night-time lip seal works best when day-time habits support it.
- Keep the nose clear. Saline rinses, allergen control, and medical treatment for rhinitis when indicated make nasal breathing easier.
- Practise a quiet nose-breathing pattern during light activity. Lips together, tongue resting on the palate, teeth slightly apart.
- Chew real food and chew it well. A fibre-rich diet gives the jaws work to do and supports muscle tone.
- Stay hydrated. Water keeps saliva moving and thins mucus, which helps nasal airflow.
- Speak with a clinician about myofunctional therapy if you struggle to maintain lip seal or tongue posture during the day.
It is easier to keep the lips together at night when this is already your default during the day.
For parents: growth, habits, and early checks
A child who keeps the mouth open at rest often has reasons, sometimes simple and sometimes needing care. Allergies, enlarged adenoids, lip or tongue ties, and habits like long-term dummy use can shift breathing and posture.
Early screening works best. Dentists and hygienists can:
- Watch for open-mouth posture, chapped lips, and drooling
- Observe tongue rest position and swallow pattern
- Ask about snoring, restless sleep, bedwetting, and morning behaviour
- Check arch width, crossbites, and spacing
An age-appropriate around-the-mouth tape, used under supervision, can help reinforce lip seal while you address causes. This tool often sits alongside myofunctional therapy and, where indicated, ENT care or orthodontic expansion.
Results you might notice
Feedback from users and clinicians tends to follow a pattern:
- Less dry mouth on waking within days
- Fewer night-time trips for water
- Reduced drooling on pillows
- Fresher breath in the morning
- A calmer, more stable tongue rest position
- In some cases, lighter snoring or fewer overnight mouth-breathing episodes
Dental markers change more slowly. Plaque scores, bleeding on probing, and caries incidence shift over months with good home care and regular visits.
Measuring progress without guesswork
Subjective change is helpful, but a few simple measures keep things grounded.
- Morning dryness rating, 0 to 10, noted weekly
- Snoring intensity tracked by a partner or a sound app
- New areas of gum bleeding during brushing, noted on a chart
- White spot lesions photographed monthly in the same lighting
- Saliva tests with your dentist for flow rate and pH, when available
- Hygienist plaque and bleeding indices at each visit
If nothing changes after eight to twelve weeks, re-check nasal patency, tape technique, and other factors like diet and reflux.
Comparing options for keeping lips together and encouraging nasal breathing
Different tools can serve a similar aim. Each has strengths and trade-offs.
| Option | How it works | Pros | Cons | Best for |
|---|---|---|---|---|
| Elastic around-the-mouth tape | Elastic ring nudges lips to meet while leaving a central opening | Gentle, less claustrophobic, easy to remove, supports habit formation | Single-use, not ideal with heavy facial hair | Most adults and supervised children who mouth-breathe |
| Straight mouth tape strip | Adhesive across the lips | Cheap, widely available | Can feel restrictive, harder to speak or cough, anxiety for newcomers | Experienced users comfortable with full lip coverage |
| Chin strap | Fabric strap supports jaw closure | Reusable, no adhesive on skin | Can shift during sleep, may not create a true lip seal, pressure marks | People with sensitive skin or adhesive intolerance |
| Myofunctional therapy | Exercises and habit training for tongue, lips, and breathing | Trains the cause, supports long-term change | Requires guidance and diligence | All ages, especially children and adults with habitual patterns |
| ENT and orthodontic care | Addresses structural or medical causes | Treats root problems like obstruction or narrow arches | Involves clinical procedures, cost, time | Those with clear anatomical or medical drivers |
The right plan often combines two or more of these.
Care and skin tips for comfortable use
Skin comfort is the main factor that makes people stop, so a little care goes a long way.
- Cleanse the area gently before use, then pat dry. Oil and residue weaken adhesive.
- If you have sensitive skin, consider a thin layer of a silicone-based barrier, applied well outside the adhesive zone, and let it dry fully.
- Rotate position slightly from night to night to avoid repeated stress on the same skin patch.
- Remove slowly, supporting the skin with fingers. A drop of warm water along the edge helps release the adhesive.
- Store tapes flat and cool. Heat can change adhesive strength.
If redness persists longer than an hour after removal, pause for a few days and speak with a clinician about alternatives.
Frequently raised questions
Is it safe to tape the mouth? An around-the-mouth design leaves a central opening and is intended to cue lip seal rather than block airflow. People with nasal obstruction, sleep apnoea, or other listed risks should seek advice first.
Will I suffocate if my nose blocks at night? You can open the mouth with a gentle push. If you wake congested, remove the tape. Treating nasal causes is part of the plan.
What if I need to cough or speak? Most users can part the lips to cough or sip water. If you need a full conversation, take the tape off and reapply later.
Can it fix crooked teeth? Taping does not move teeth. It supports a healthier environment and better muscle patterns, which can stabilise orthodontic results and reduce relapse risk when combined with proper treatment.
How long before I notice changes? Comfort can improve within days. Changes in morning dryness and breath often show within a week or two. Dental markers take months, and they depend on diet and hygiene.
Is it safe during a cold or hay fever flare? If the nose is blocked, skip taping. Focus on nasal care and return to taping when breathing through the nose feels easy again.
A practical workflow for dental teams
Clinicians can fold lip seal support into routine care without extending chair time.
- Ask two screening questions: Do you wake with a dry mouth? Does anyone say you snore with your mouth open?
- Observe lip posture at rest during the medical history and in the chair.
- Record plaque and bleeding indices, and note areas with chronic dryness or irritation.
- Offer a short explanation of saliva’s role and how open-mouth breathing disrupts it.
- Demonstrate an around-the-mouth tape during the visit. Apply for five minutes while discussing home care.
- Provide a written plan with a 4 to 8 week trial, plus nasal care advice and a simple diary.
- Arrange review, with metrics that include morning dryness rating and bleeding sites.
Hygienists are well placed to lead this, and orthodontists working with children may integrate taping alongside expansion and habit training.
Bringing it together with daily habits
Consistency keeps gains. Pair lip seal at night with a few steady habits:
- Brush twice daily with a fluoride paste, spit, and do not rinse
- Use interdental brushes or floss once a day
- Keep sugars with meals and keep frequency low
- Rinse the nose with saline on days when pollen or dust flare
- Chew sugar-free gum after meals to stimulate saliva
- Keep a water bottle handy and sip through the day
The small changes add up.
Quick-start checklist
- Patch-test the adhesive in the day
- Prepare skin, dry completely, trim hair if needed
- Practise while awake for 10 to 15 minutes
- Use during the first half of the night for a few days
- Track morning dryness once a week
- Note any snoring changes reported by a partner
- Review after four weeks and adjust with your dental team
A quiet nose, lips that meet easily, and a mouth that wakes up feeling fresh are good signs that you are moving in the right direction.


















0 comments