Every day, clinicians see the signs of chronic mouth breathing written across the dentition and soft tissues. Dry, fissured lips. Inflamed gingivae that never quite settle. Relapse in cases that should be stable. Parents worried about restless sleep and narrow palates. The airway links all of it, and a simple change in habit can move the needle for many patients. One tool that has gained traction in dental circles is MyoTape, a lip-rest training aid that promotes nasal breathing without sealing the lips shut.
It is not a magic fix. It is a prompt, a coach patients can wear, and a way to translate chairside advice into nightly action.
Why nasal breathing matters to dental teams
Nasal breathing supports oral and general health through mechanics and chemistry. It filters, warms and humidifies air, and it encourages diaphragmatic patterns rather than upper-chest huffing. For the mouth, the spider web of effects is hard to ignore.
- Saliva remains less viscous, buffering acids more effectively
- pH stays more stable, which may slow demineralisation
- Gingival inflammation often reduces when lips are closed during sleep
- Orthodontic outcomes tend to settle better with a healthy lip seal and tongue posture
- Snoring and fragmented sleep frequently improve, which helps daytime function and behaviour in children
- Less nocturnal mouth opening means fewer dry-mouth complaints and fewer cracked commissures
Mouth breathing pulls the system in the opposite direction. Evaporative stress dries tissue, caries risk rises, plaque matures faster, and many patients grind or clench more when the airway feels precarious. Early airway care can change growth patterns in children and can protect restorative and orthodontic work in adults. The mouth mirrors the airway every night.
What MyoTape is and how it works
MyoTape is an elastic, skin-safe adhesive tape that sits around the lips rather than across them. The centre remains open. The elastic pulls inward, cueing the lips to meet. The wearer can still part the lips if needed, cough, or speak. The aim is habit training, not forced closure.
Three things happen when patients use it correctly:
- Proprioceptive input increases. The skin around the mouth senses the pull toward closure.
- Gentle elastic tension helps the lips rest together with less effort.
- Nasal airflow increases by default, which can improve nitric oxide exposure and humidity.
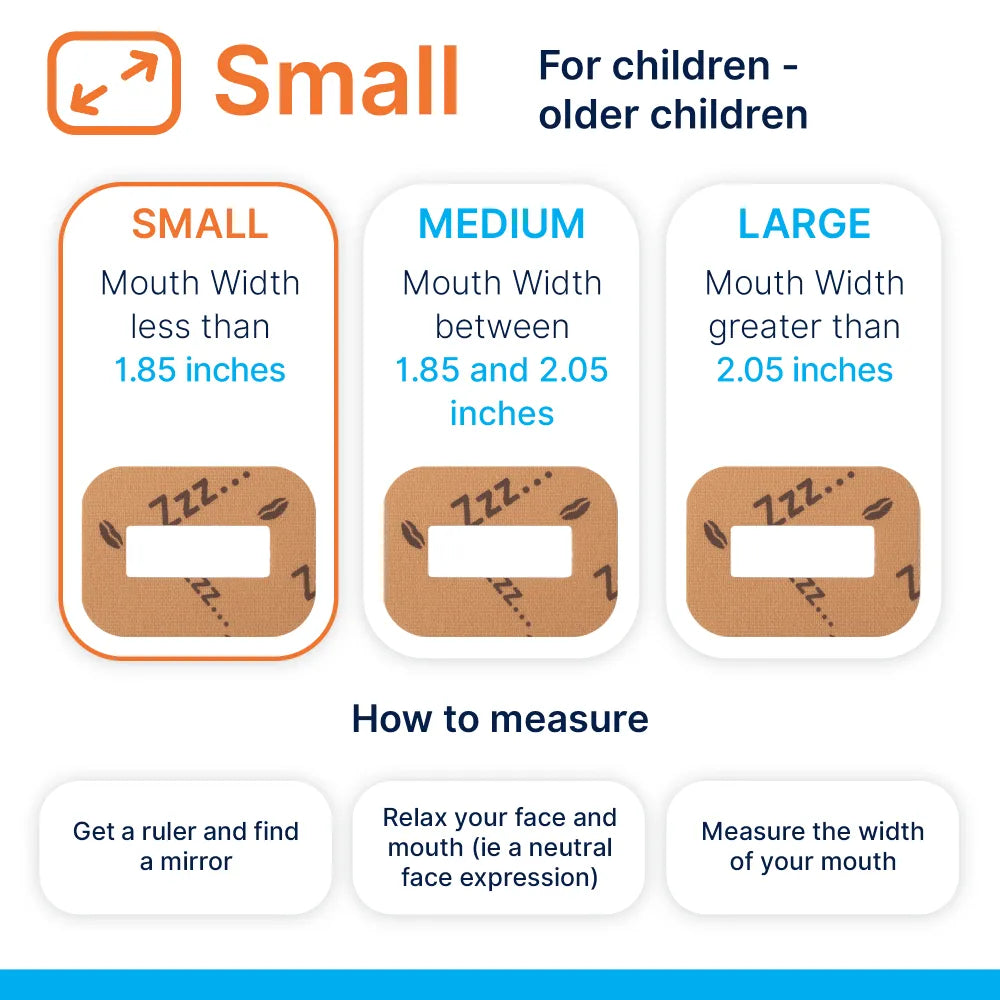
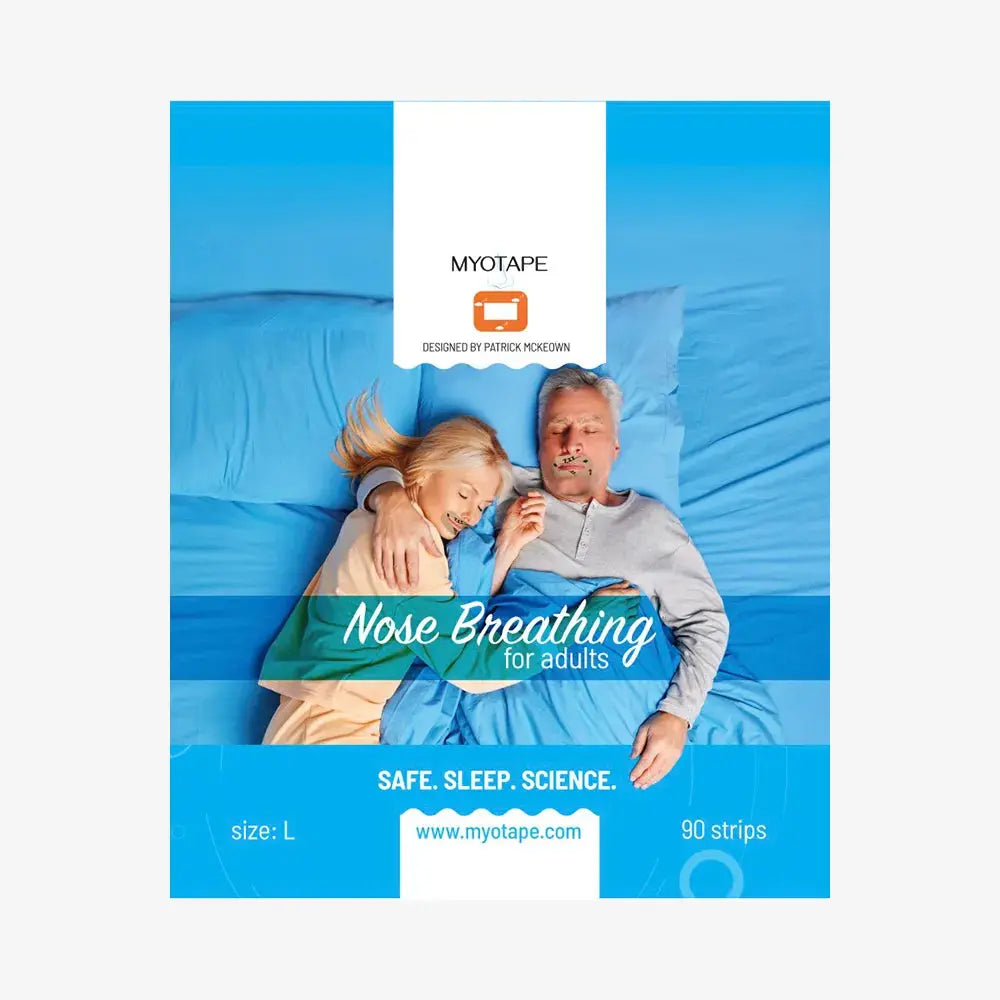
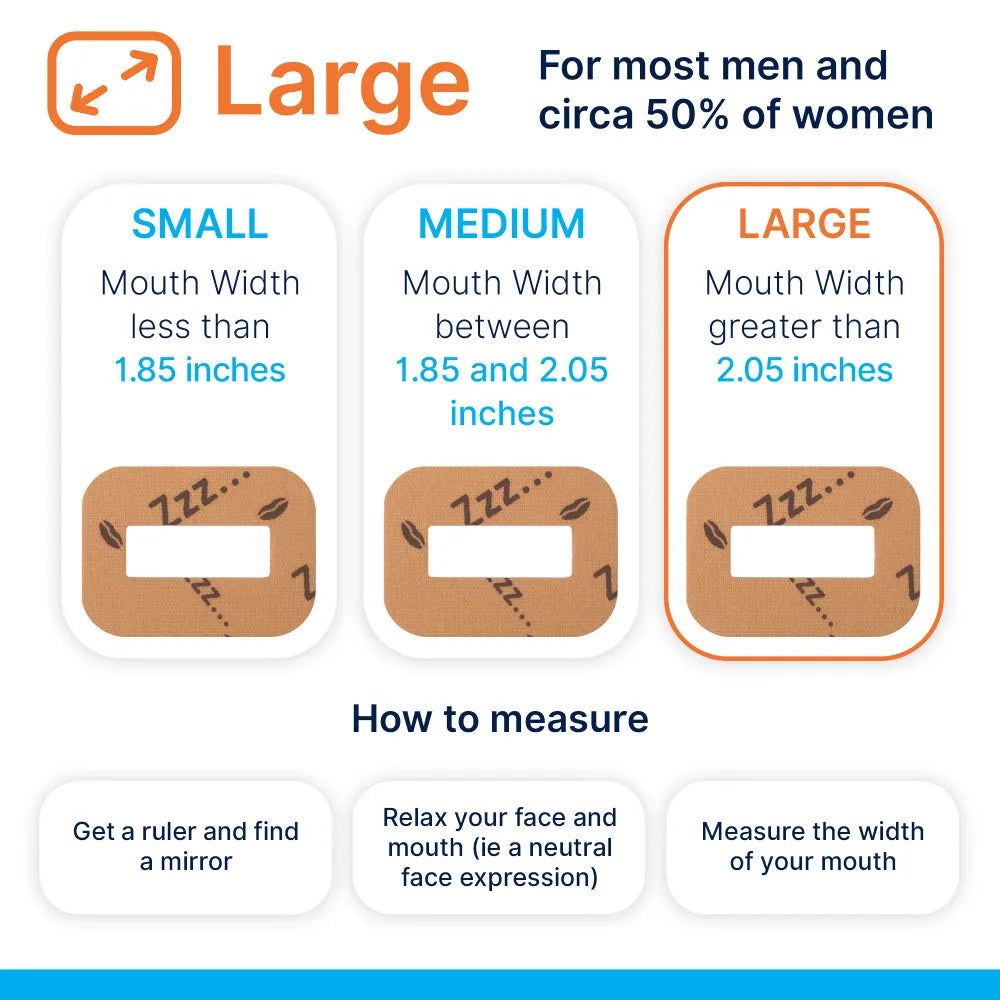
The material is usually hypoallergenic cotton with a medical-grade adhesive. Sizes are available for adults and for children. If the patient has facial hair, placement can be tricky and may require trimming for good contact.
Who should not use it:
- Anyone with current nasal obstruction that prevents easy nose breathing
- Those with vomiting or reflux that is poorly controlled
- Patients with diagnosed moderate to severe sleep apnoea who are not yet managed
- Individuals with active respiratory infection
- Anyone with a known allergy to adhesives or open perioral skin conditions
Children should only use it under adult supervision and with clinician guidance. Patients with doubts about safety should trial it while awake before any overnight use. If nasal breathing is difficult during a relaxed five-minute daytime test, do not recommend overnight use until the nose is clear.
Where it fits in a care pathway
MyoTape belongs inside a broader airway-led approach. It is one piece in a plan that starts with screening, moves through education and simple exercises, and may lead to referrals.
Suggested flow:
- Screen every new patient and recall for mouth breathing, snoring, and daytime fatigue
- Check nasal patency, septal deviation, turbinates, and mouth posture at rest
- Use brief questionnaires like the NOSE scale, Epworth Sleepiness Scale, or the short STOP screen
- Assess tongue posture, lip tone, and swallow
- Provide nasal hygiene advice and simple breathing drills where appropriate
- Introduce MyoTape as a nightly cue once nasal breathing is comfortable
- Reassess outcomes and adapt the plan
In orthodontics, tape can stabilise a new lip seal alongside arch development and myofunctional work. In periodontics, it can lower nocturnal dryness and reduce gingival irritation for certain patients. In restorative care, it can protect the environment around new work.
Implementation steps for a dental practice
Getting this right requires a protocol. The clinical steps are straightforward, but clarity keeps patients safe and results consistent.
- Create a one-page airway screening form
- Build a standard script for explaining nasal breathing and lip seal
- Stock multiple sizes of MyoTape and note batch numbers in records
- Add a short consent specific to habit-training aids
- Train the team on application, removal, and troubleshooting
- Provide written home instructions with images
- Set a review point at two weeks, then six weeks, then three months
Record metrics before and after:
- Self-reported dry mouth upon waking
- Partner reports of snoring or mouth breathing
- Plaque scores and BOP
- White spot monitoring around brackets
- Orthodontic stability notes
- Patient-reported sleep quality
Small wins add up. A patient who reduces mouth opening for half the night already gains ground.
Clinical scenarios
Case 1: Early orthodontic crowding in a nine-year-old
Narrow arches, anterior open lip posture, and dark under-eye shadows. NOSE score 35. The practice used nasal hygiene advice, tongue-to-spot posture drills, and a slow maxillary expander. MyoTape was introduced after two weeks of improved nasal airflow. Parents reported quieter sleep within days. Three months later, the lip seal at rest was consistent and the expansion held with less relapse pressure.
Case 2: Adult bruxism and morning headaches
A 37-year-old with polished facets, recurrent chips, and nightguard marks that suggested clenching. Snoring on back sleeping only, Epworth 7, BMI normal. After a negative screen for significant apnoea, the plan focused on nasal breathing, stress reduction, and MyoTape as an overnight cue. Dry-mouth complaints faded within a week. Clenching reduced according to the patient and partner, and nightguard wear decreased. The patient continued periodic use when travelling or under stress.
Case 3: Peri-implant bleeding and xerostomia
A 62-year-old on multiple medications with low resting saliva and morning soreness. Mouth breathing at night was clear. The team paired saliva support measures with staged reintroduction of nasal breathing. MyoTape was added after saline rinses and a short trial of nasal strips improved comfort. Bleeding scores fell across three maintenance visits. The patient valued the subjective comfort most of all.
Evidence snapshot
The research on mouth taping is growing but still modest in size. Studies on snoring and mild sleep-disordered breathing show reductions in snoring frequency and intensity when the mouth is gently kept closed. Small trials indicate a drop in apnoea events in selected adults when taping is combined with positional strategies and nasal support. For children, the strongest base still sits with myofunctional therapy, arch development, and ENT care when needed. Taping acts as an adjunct that makes good habits more likely at night.
Mechanistically, nasal airflow increases nitric oxide exposure and humidity, which may benefit airway tone and mucosal health. Reduced evaporative loss protects saliva function. Orthodontic stability tracks with improved lip seal and tongue posture.
Realism matters. MyoTape will not fix severe apnoea. It does not replace CPAP. It is a low-risk prompt that can support a plan and give predictable gains in specific groups.
| Clinical area | What the literature suggests | Quality of evidence | Practical expectation |
|---|---|---|---|
| Snoring in mild cases | Lower frequency and volume in many users | Small RCTs and cohorts | Noticeable improvement for partners in a few nights |
| Mild sleep-disordered breathing | Modest AHI reduction in selected adults with nasal patency | Limited trials | Helpful adjunct with screening and follow-up |
| Orthodontic stability | Better lip seal supports arch form retention | Indirect and observational | Cleaner soft tissue patterns and fewer relapse triggers |
| Caries and perio risk | Less dryness and more stable pH overnight | Mechanistic and clinical observation | Lower morning plaque maturation and irritation |
| Paediatric growth patterns | Benefits strongest with full airway and ortho-myofunctional plans | Mixed, growing base | Better sleep quality and rest posture over months |
Invite curiosity, apply clinical judgement, and track outcomes in your own audit cycle.
Frequently asked questions your patients will ask
Is it safe?
For healthy nasal breathers, yes, when used as directed. The lips can part if needed. Start with a daytime trial while reading or watching TV.
Will I suffocate if my nose blocks at night?
The centre of the tape is open and the lips can separate. If your nose tends to block, address that first with nasal care or medical advice. Only use MyoTape once the nose is clear.
Does it stop snoring?
Many partners report less snoring. It helps most when the noise comes from mouth breathing rather than deep airway collapse.
Can it replace my CPAP?
No. It may improve comfort with CPAP by reducing mouth leak, but do not stop prescribed therapy without medical guidance.
What about skin irritation?
Most people tolerate the adhesive well. Apply on clean, dry skin, avoid creams on the area, and remove slowly. If redness persists, take a break and speak to your clinician.
Can children use it?
Yes, with adult supervision and only after a clinician confirms nasal breathing is comfortable. Start with short periods while awake.
How long before I notice change?
Some feel immediate relief from dryness. Snoring changes are often seen within a week. Habit change for lips and tongue can take a few months.
Risk management and consent
A written protocol helps everyone. Keep a clear decision tree in the notes.
- Document airway screens, nasal patency, and any red flags
- Gain consent that covers the habit-training nature of the product and the plan
- Provide a safety sheet that lists when to stop use: blocked nose, illness, new skin reaction, or any breathing concern
- Refer to ENT if signs suggest turbinate hypertrophy, septal deviation, chronic rhinitis, or adenoidal issues
- Refer to a sleep physician if screening suggests moderate to severe apnoea
- Reinforce that this does not replace medical treatment
A short audit every quarter keeps the team sharp. Track adverse events, patient feedback, and clinical metrics.
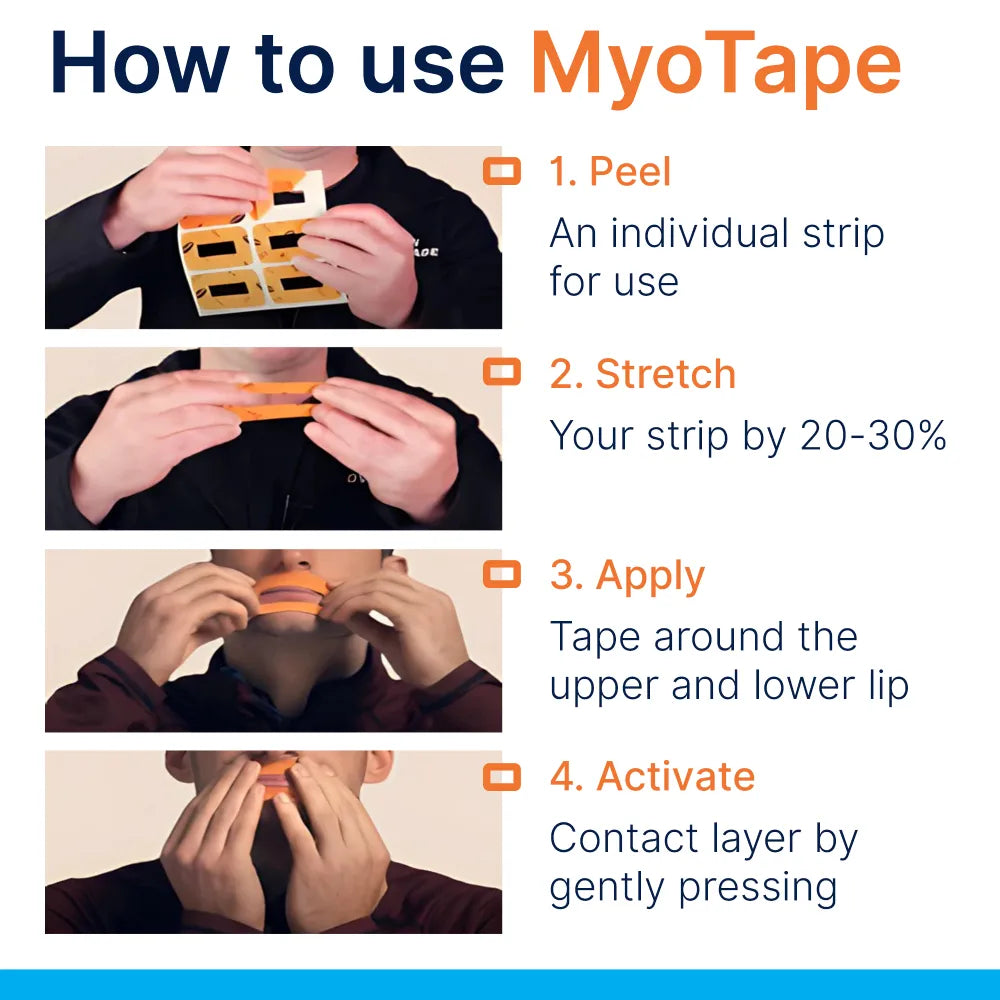
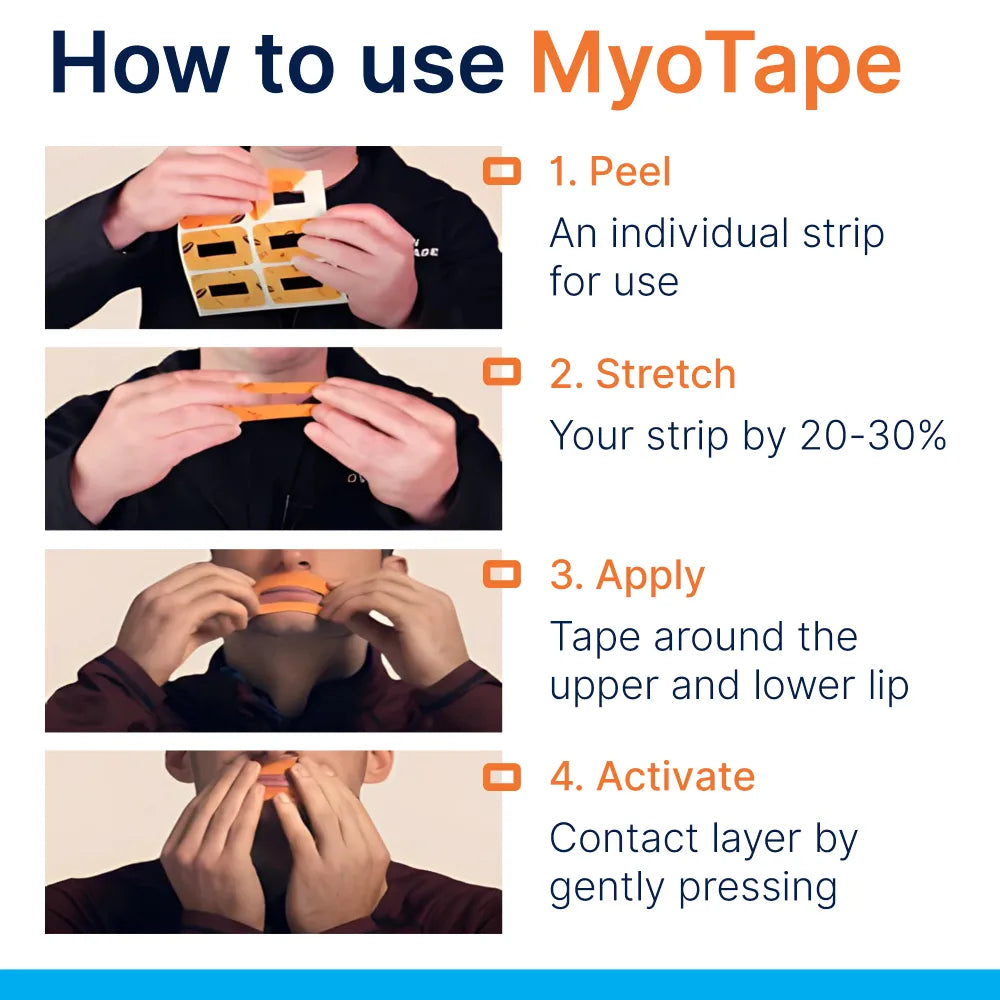
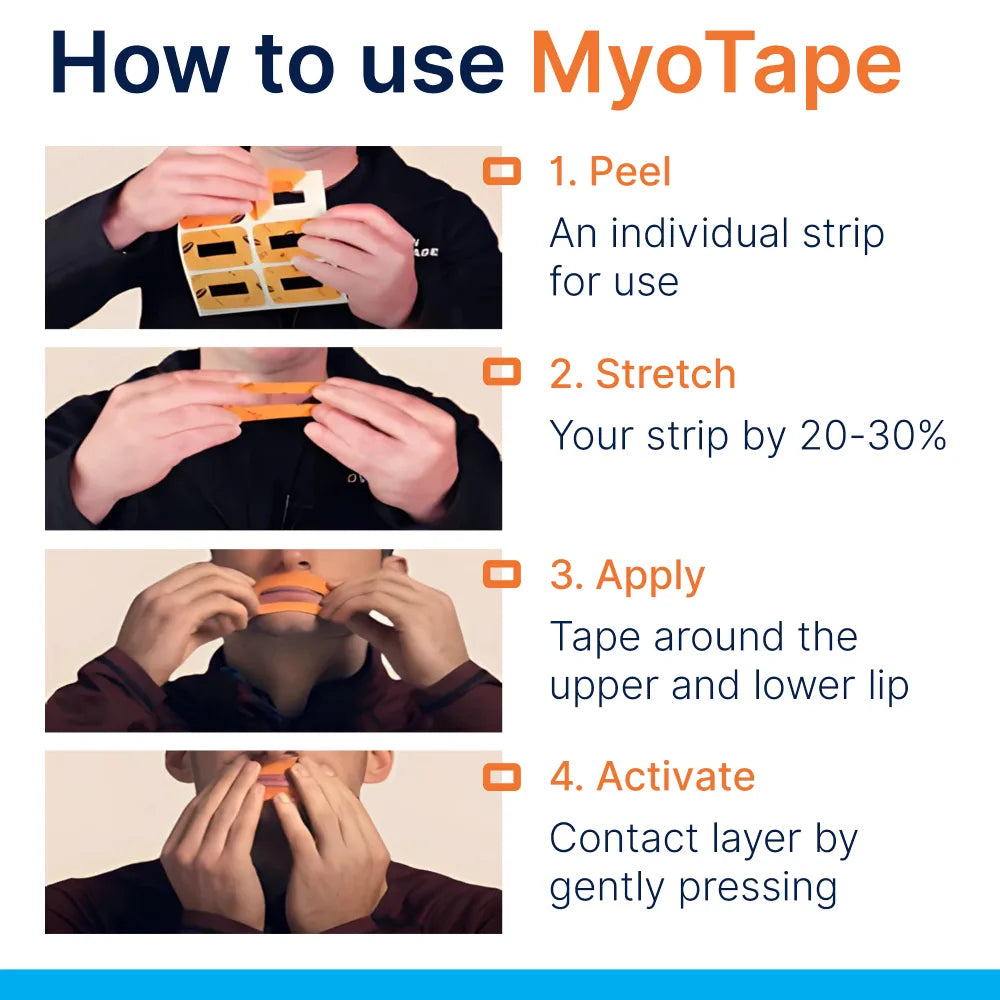
Step-by-step guide you can share with patients
- Clean and dry the skin around your lips
- Sit or lie comfortably and relax your jaw
- Place the tape so the opening sits over the lips, not across them
- Lightly lick and seal your lips, then let the elastic help them meet
- Breathe gently through your nose for five minutes while awake
- If comfortable, wear for a short nap or the first part of the night
- Build up to all-night use over a week
- Remove by supporting the skin with one hand and peeling slowly with the other
- Stop use if your nose blocks, you feel unwell, or the skin becomes sore
Pair this with simple drills:
- Tongue-to-spot: keep the tip on the incisive papilla during light nasal breathing
- Lip holds: press lips together lightly for 10 seconds, relax for 10 seconds, repeat ten times
- Nasal care: saline rinse in the evening if dryness or congestion is common
Stocking, pricing, and ROI for the practice
MyoTape is inexpensive, easy to store, and quick to teach. It fits naturally into ortho reviews, perio maintenance, airway consults, and hygiene visits. Packaging one month of tape into a home kit with instructions can lift adherence and reduce follow-up calls.
Ways to offer it:
- As part of a paediatric airway starter kit with nasal care and habit guidance
- Bundled into orthodontic retention plans
- Included with hygiene plans for patients who report dry-mouth mornings
- Used during CPAP mask fitting for patients with leak issues in joint clinics
Indicative numbers:
- Wholesale cost per unit: low single digits in pounds
- Retail fee for a one-month kit with coaching: covers staff time and follow-up
- Potential savings: fewer emergency visits for cracked lips or sore tissues, improved stability in ortho, better patient satisfaction scores
Keep it ethical. Position it as a tool that supports a larger plan, not a cure-all.
Training and team development
Confidence grows with shared language and practical drills. A short in-house workshop can raise the standard quickly.
Suggested agenda:
- Airway basics for dental teams
- Chairside screening without extra appointment time
- Safe introduction of MyoTape and patient selection
- Myofunctional basics: tongue posture, swallow, lip seal
- Referral pathways to ENT, sleep medicine, and allied therapists
- Audit methods and patient-reported outcomes
Useful learning routes include myofunctional therapy courses, sleep dentistry modules, and ENT-led workshops on nasal patency. Pair theoretical learning with a few pilot cases to build local know-how.
What success looks like at 3, 6, and 12 months
Three months
- Patients report less morning dryness and fewer cracked lips
- Partners notice quieter nights
- Plaque control improves where dryness was a barrier
- Early ortho retention feels more stable
Six months
- Lip seal looks effortless at rest
- Tongue posture is more consistent
- Snoring episodes drop further for many cases
- Maintenance visits show calmer gingivae
Twelve months
- Fewer relapse triggers in ortho and fewer failed bondings
- Lower rates of night-time mouth breathing based on partner logs
- Stronger patient buy-in for airway-first care
- A steady stream of referrals from grateful families
Chairside checklist for the next patient who mouth breathes at night
- Ask: Do you wake with a dry mouth? Do you snore? Do you wake often?
- Look: lip incompetence at rest, anterior open lips, scalloped tongue, narrow palate
- Test: can the patient nasal breathe comfortably for five relaxed minutes?
- Record: NOSE score, Epworth, plaque and BOP baselines
- Teach: tongue-to-spot, gentle nasal breathing, simple nasal hygiene
- Trial: short daytime use of MyoTape, confirm comfort and safety
- Supply: right size tape, written instructions, and warnings
- Review: two weeks, six weeks, then three months
- Refer: ENT or sleep physician if screens or symptoms warrant it
Small habits, repeated nightly, protect a lifetime of dental work. MyoTape gives patients a nudge in the right direction and gives dental teams a practical way to support better sleep, better saliva, and calmer tissues.


















0 comments