Many people have heard about taping the mouth at night to encourage nasal breathing, yet are unsure what that might mean for oxygen levels while asleep. Questions usually sound like this: will I suffocate, will my oxygen drop, or could it actually help? The short answer is that for the right person, used properly, it can help nose breathing and reduce mouth leaks. Oxygen levels mainly improve when mouth taping reduces airway collapse or stabilises breathing. There are limits though, and safety matters.
Let’s look at how oxygen behaves overnight, why nasal breathing is different to breathing through the mouth, and where a purpose built product like Myotape fits in.
Why nasal breathing can help night time oxygenation
Nasal breathing filters, warms and humidifies air, which keeps the airway calmer and less irritable. The nose also produces nitric oxide that mixes with inhaled air. Nitric oxide relaxes blood vessels in the lungs and can support better matching between airflow and blood flow. This can lead to more efficient oxygen transfer.
There is a mechanical piece too. Breathing through the nose encourages the tongue to rest on the palate and activates the diaphragm. Both effects support a more open upper airway once you fall asleep. A more stable airway means fewer collapses, quieter breathing and, in many cases, fewer dips in oxygen.
Mouth breathing tends to dry tissues and bring the jaw backwards. That makes the throat more collapsible. In people with snoring or obstructive sleep apnoea, this can translate into more frequent pauses or flow reductions, which is when oxygen drops.
What mouth taping products try to achieve
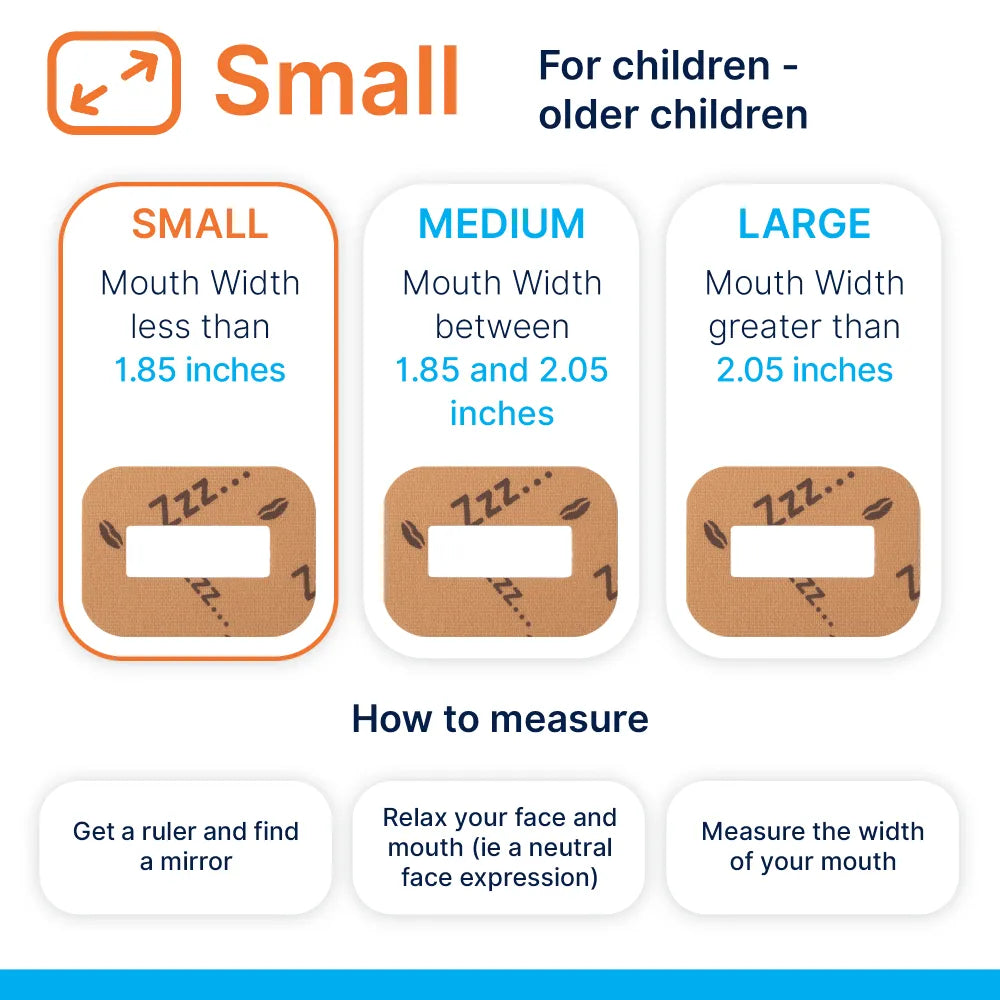
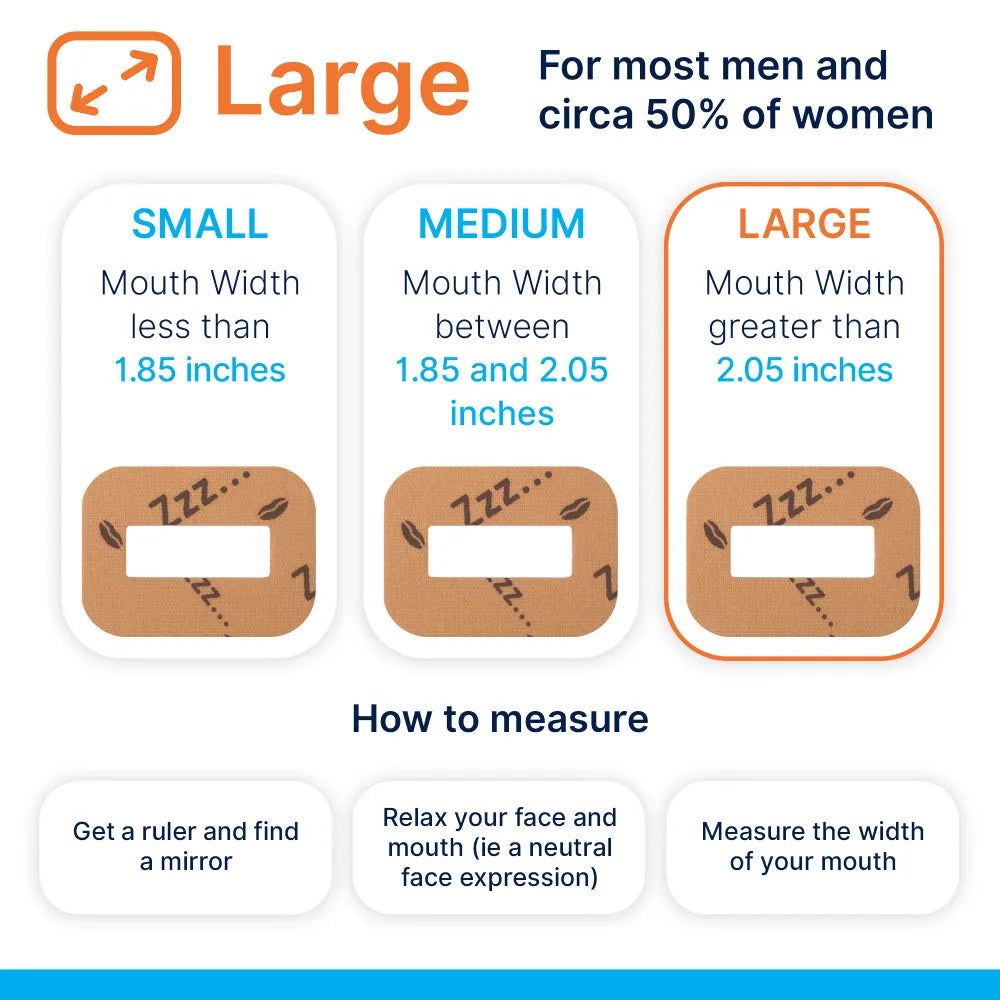
People sometimes use ordinary tape across the lips, which can feel harsh and unsafe. Myotape is designed differently. It sits around the mouth and gently encourages the lips to stay together while leaving a small central gap. You can still part your lips in a pinch. The goal is not to glue the mouth shut, but to remind the body to use the nose.
That distinction matters for safety and comfort. A softer adhesive, a breathable textile and a design that keeps an opening available all reduce risk. The product is essentially a trainer for lip seal rather than a lock.
What we know from research so far
Evidence is growing but still modest. Small pilot studies suggest that taping the mouth in people with primary snoring or mild obstructive sleep apnoea can reduce snoring and may lower the number of breathing events. Some reports in CPAP users show improved mask seal when mouth leaks are reduced, which in turn can stabilise oxygen.
There is no high quality proof that mouth taping treats moderate or severe sleep apnoea on its own. In those cases, therapies like CPAP or a mandibular advancement device have much stronger evidence for normalising oxygen levels and protecting long term health. Mouth taping may still help with symptoms in selected situations, but it should not replace proper treatment where that is needed.
Oxygen metrics that actually matter at night
A fingertip oximeter gives a headline percentage, yet clinicians look at patterns. The following markers help you make sense of your own data.
- Baseline SpO2 during sleep: many healthy adults sit between 94 and 97 percent, a little lower than daytime.
- Nadir SpO2: the lowest reading of the night. Brief dips to the low 90s can appear in healthy sleep, but repeated dips below 90 percent point to a problem.
- Oxygen Desaturation Index, often called ODI: how many times per hour oxygen drops by at least 3 or 4 percent from baseline.
- Time below 90 percent, sometimes written T90: the total minutes spent at or under 90 percent.
- Coupling with breathing events: in a sleep study, desaturations linked to apnoea or hypopnoea carry more weight than random artefacts.
If you trial any intervention, watch trends in ODI, nadir and T90, not just a single nightly average.
Ways to measure your night time oxygen
Different tools suit different questions. Here is a quick comparison.
| Method | What you get | Strengths | Limitations |
|---|---|---|---|
| Spot check fingertip oximeter | Live SpO2 and heart rate | Affordable, easy to use | No overnight trend unless it records, can slip and create artefacts |
| Recording pulse oximeter | Full night SpO2 trace, ODI, T90 | Clear pattern of desaturations, exportable reports | Motion artefacts, less context about airflow or snoring |
| Wearable ring or watch with FDA or CE marking | Trend data, estimated desats, sometimes snoring | Comfortable, long term trends | Algorithms vary, may miss brief events |
| Home sleep apnoea test | Airflow, effort, oxygen, position, snoring | Links desats to events, clinician report | One or two nights, access needed |
| Full polysomnography | Brain waves, muscle tone, breathing, oxygen, arousals | Gold standard, explains sleep quality and breathing together | Costly, waiting lists, lab environment |
| CPAP machine data | Leak, AHI, sometimes SpO2 with add ons | Shows impact on treated breathing and leaks | No oxygen without extra sensor, applies only to CPAP users |
No single device answers everything. Pick the tool that matches your level of concern and the decisions you need to make.
How Myotape could influence oxygen levels
There are several plausible mechanisms.
- Reduced mouth leak: in nasal mask or nasal pillow CPAP users, mouth leak can dilute pressure, leading to residual events and desats. Encouraging lip seal can cut leak and improve oxygen stability.
- Better airway shape: a closed mouth supports tongue posture and jaw position, which may reduce collapsibility in light sleep.
- Nitric oxide advantage: air through the nose carries locally produced nitric oxide that can support gas exchange in the lungs.
- Breathing chemistry: breathing through the nose tends to be slightly slower and quieter, which can stabilise carbon dioxide within a healthy range. Stable carbon dioxide helps regulate respiratory drive during sleep.
These gains depend on your baseline issues. If desaturations come from significant airway collapse due to anatomy or high loop gain, tape alone will not fix it. If mouth leaks or habitual mouth breathing are the main triggers, tape can be helpful.
Who might benefit, and who should avoid it
People who might benefit
- Habitual mouth breathers without severe nasal blockage
- Primary snorers and those with mild sleep apnoea who prefer conservative steps first
- CPAP users with good pressure but persistent mouth leak and dry mouth
- Those with allergies who have done the basics for nasal care and still open the mouth at night
People who should not use mouth tape unless cleared by a clinician
- Known moderate to severe obstructive or central sleep apnoea not on treatment
- Chronic respiratory disease with resting or nocturnal hypoxaemia
- Significant nasal obstruction, severe deviated septum or acute sinus infection
- Gastro-oesophageal reflux with frequent night time vomiting or regurgitation
- Skin conditions around the mouth, adhesive allergy, open sores
- Recent facial surgery or trauma
- Panic disorder, severe claustrophobia, or anyone who feels unsafe with tape
- Children unless using a product designed for paediatric use under professional guidance
- Anyone who has consumed alcohol to excess or sedatives that night
If you are unsure which group you belong to, speak with your GP or a sleep professional first. Safety comes first.
A practical set up guide
The idea is to make nasal breathing easy and mouth taping a light touch reminder. Prepare first, then apply.
Nasal preparation
- Rinse the nose with saline in the evening if you feel congested.
- Use any prescribed nasal steroid regularly, not just on the night you tape.
- Keep the bedroom air slightly humid, especially in winter.
Skin preparation
- Clean and dry the skin around the mouth, avoid heavy moisturisers right before bed.
- Patch test the adhesive on your inner forearm during the day to check for irritation.
- Trim facial hair near the corners of the mouth to help adhesion if needed.
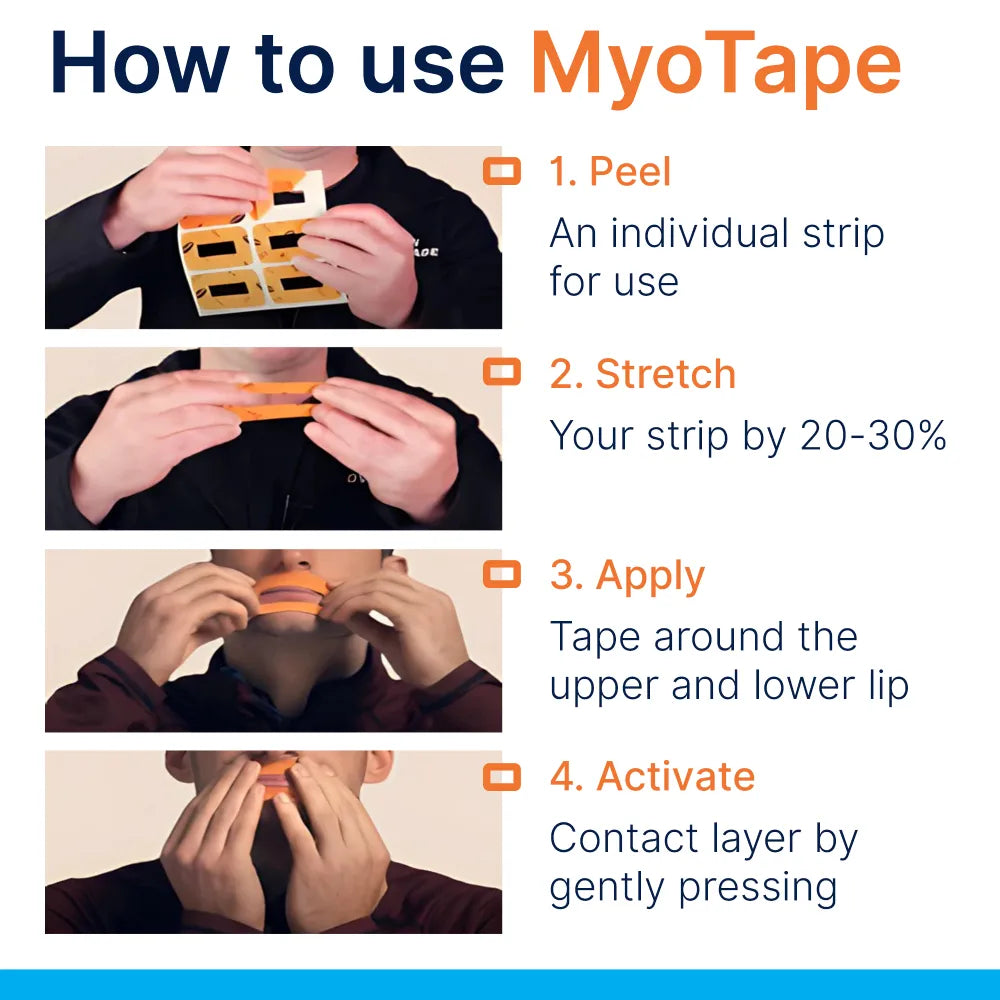
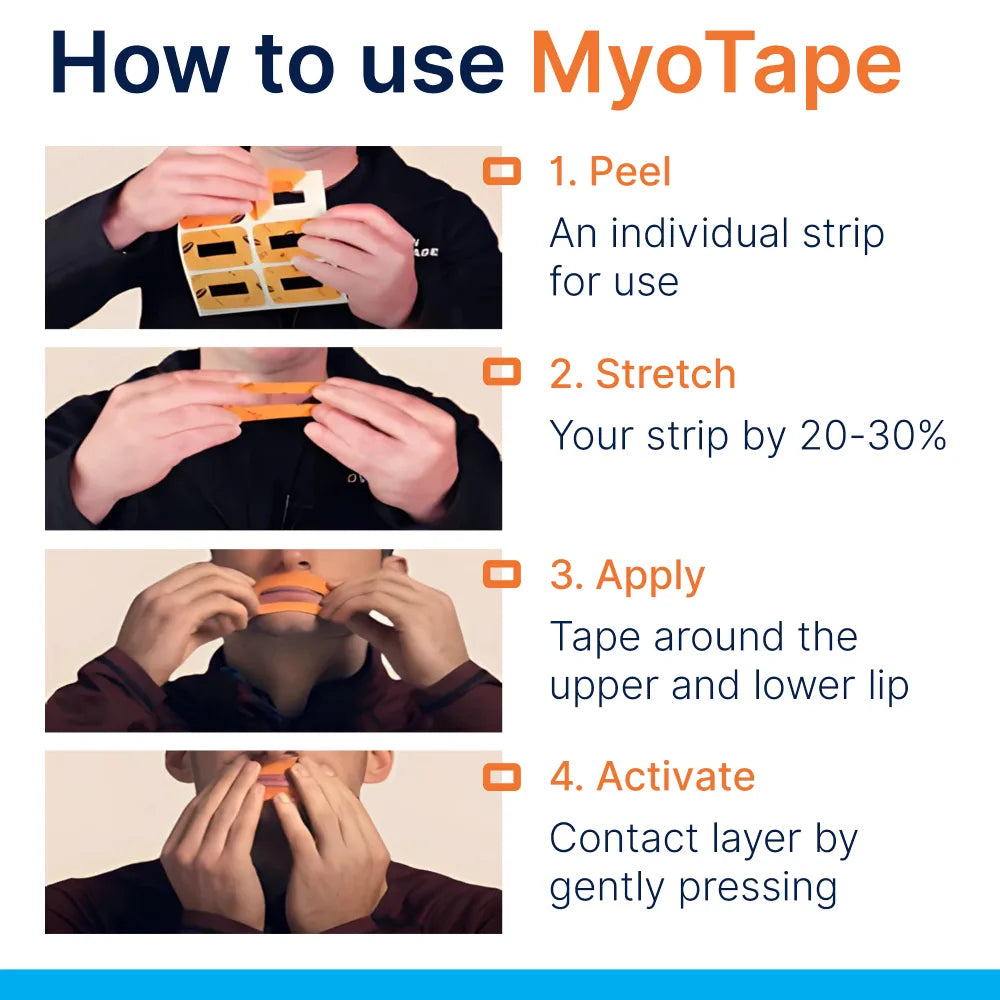
Applying Myotape
- Sit upright. Centre the tape so the opening aligns with your lips.
- Apply the bottom part first, then the top, smoothing the sides around the mouth.
- Keep a small bowl of water and small scissors on the bedside table, which can help loosen or cut the tape quickly if needed.
- Try five minutes while reading in the evening to get used to the feel.
- Only use at night when you can breathe freely through the nose.
Stop immediately if you feel short of breath, panicky, or unwell.
Setting expectations
If mouth leaks or mouth breathing are the problem, you may notice quieter breathing, less dry mouth and fewer awakenings. Some people see fewer oxygen dips on a recording oximeter. Others feel no change, which suggests a different cause needs attention.
Improvements often appear alongside other simple steps:
- Side sleeping or anti supine strategies
- Weight reduction if needed
- Avoiding alcohol within three hours of bedtime
- Treating nasal allergies consistently
- Nasal dilators or Breathe Right strips to lower nasal resistance
- Tongue and orofacial exercises that support lip seal and tongue posture
- Reviewing medications that may worsen congestion or relaxation
Myotape is one tool. It tends to work best when the nose is clear and sleep timing is regular.
Common questions
Will carbon dioxide build up? Mouth taping does not block airflow if the nose is clear and an opening remains available. Nose breathing can slightly increase carbon dioxide toward a healthy range, which usually stabilises breathing rather than causing harm. If you cannot breathe comfortably through your nose, do not tape.
Could oxygen drop if my nose blocks suddenly? If you have unpredictable congestion, use a highly breathable design with a central gap, and only on nights when the nose is clear. Some people set a low alarm on a recording oximeter during a trial. If you wake with breath hunger or see significant desaturation, stop and seek advice.
Is ordinary tape the same? No. Hardware tape can irritate the skin, seal too aggressively and feels unsafe to many. A product created for the face with a central opening, gentle adhesive and elastic fabric is more forgiving.
What about dental work or dentures? If your dental appliance alters lip seal or jaw posture, speak with your dentist. Many people use mouth taping with retainers or aligners without issue, but the fit and saliva flow matter.
Pregnancy and mouth taping? Avoid self directed experiments in pregnancy without checking with your midwife or GP. Nasal congestion can be common in pregnancy and may make taping uncomfortable.
Can children use it? There are versions designed for children, often used under guidance for mouth breathing habits. Assessment for adenoids, tonsils and nasal issues is sensible first.
A two week trial plan you can follow
This plan suits adults with mild snoring or suspected mild sleep apnoea who can breathe through the nose and have no red flags.
Before you start
- Keep a simple sleep diary for three nights. Note snoring reports, awakenings, morning dry mouth and energy.
- If you can, record overnight oxygen with a ring or fingertip device that saves data.
- Prepare the nose and skin as described above.
Week 1
- Night 1: wear Myotape for 20 to 30 minutes while reading. Remove before sleep.
- Night 2 to 3: wear for the first sleep cycle, which is often 90 minutes. Remove if you wake and feel uneasy.
- Night 4 to 7: wear through the night if comfortable. Keep water and scissors at the bedside.
Week 2
- Continue nightly use if comfortable. Record oxygen on two of the nights.
- Add one supportive change, for example a nasal dilator or side sleeping wedge.
What to track
- Snoring volume and pattern, using a smartphone app or partner reports
- Dry mouth on waking, rated 0 to 10
- Awakenings and sleep quality
- Any oxygen metrics you can collect, especially nadir and ODI
- CPAP users should note leak rates and residual AHI
When to stop early
- Any sense of struggling for air
- Oxygen dips that are new or worse than baseline
- Skin irritation that does not settle with a rest day
- New chest symptoms or severe nasal blockage
What a good response looks like
- Quieter snoring, fewer mouth leaks, reduced dry mouth
- ODI lower, nadir a little higher, less time below 90 percent
- More continuous sleep and better alertness
If there is no change, consider alternative or additional steps, and speak with a sleep clinician if symptoms persist.
Combining with CPAP or oral appliances
CPAP
- If you use a nasal mask and have high leak, Myotape can reduce leak and raise effective pressure at the airway.
- Check your machine’s leak data after a week of use. Expect fewer large leak flags and fewer residual events.
- Keep your pressure settings unchanged during a short trial unless your clinician advises otherwise.
Oral appliances
- Mandibular advancement devices pull the jaw forward, which opens the airway. Pairing with lip seal can further limit mouth opening and snoring, but comfort varies. Trial on a weekend first.
Fine tuning the nose
A clear nose is the main predictor of success.
Practical steps
- Daily saline rinse in the evening during allergy season
- Consistent use of prescribed nasal steroid sprays, with correct technique angled slightly outward
- Allergen control in the bedroom, like encasing pillows and regular hot washing of bedding
- Evaluate for structural issues if one side of the nose is always blocked
If the nose is comfortable and breathing is quiet, mouth taping feels almost redundant. That is the sweet spot.
When oxygen levels keep dipping
Persistent desaturations point to causes that mouth taping cannot resolve on its own. Clues include loud disruptive snoring, witnessed apnoeas, morning headache, spikes in blood pressure, frequent urination at night and daytime sleepiness. In those cases, ask your GP for a sleep assessment. Formal treatment can make a marked difference to health, mood and blood pressure, and you can still use adjuncts like Myotape for comfort or leak control with professional oversight.
Where to go next for tailored advice
- Your GP can arrange a home sleep apnoea test or refer you to a sleep clinic.
- A registered sleep physiologist or respiratory therapist can help interpret oximetry and CPAP data.
- A dentist trained in sleep medicine can advise on oral appliances and jaw posture.
- A physiotherapist or myofunctional therapist can guide tongue and orofacial exercises that support nasal breathing and lip seal.
Used thoughtfully and safely, encouraging nasal breathing at night can support quieter sleep and, for some, steadier oxygen. The key is matching the tool to the problem, preparing the nose, and checking objective data rather than guessing.













0 comments