Sleep can feel like a moving target when breathing is part of the problem. Many people read about mouth taping and wonder if a simple strip of tape could quiet snoring, steady breathing, and leave them feeling sharper during the day. Among the options available, Myotape has gained attention because it sits around the lips rather than sealing them shut, encouraging the mouth to stay closed while still allowing speech and a quick sip of water. That nuance matters when the subject is sleep apnoea.
This guide looks at how Myotape fits into care for snoring and obstructive sleep apnoea, what the evidence suggests, who it might help, who should avoid it, and practical steps for trying it safely. Nothing here replaces advice from a sleep clinician, but it can help you ask sharper questions and make informed choices.
What mouth taping tries to change
When we sleep with the mouth open, the jaw falls back and the tongue follows, the throat dries out, and turbulence rises. The airway becomes more likely to narrow or close. Nasal breathing does the opposite. It warms, filters, and humidifies air, supports more stable breathing chemistry, and helps maintain tongue posture against the palate.
Mouth taping aims to nudge the system toward nasal breathing for more of the night. That can reduce snoring volume in some people and may lower the number of breathing events in those with mild obstructive sleep apnoea. It is not a cure, and it is not a substitute for proper diagnosis.
How Myotape differs from standard lip tape
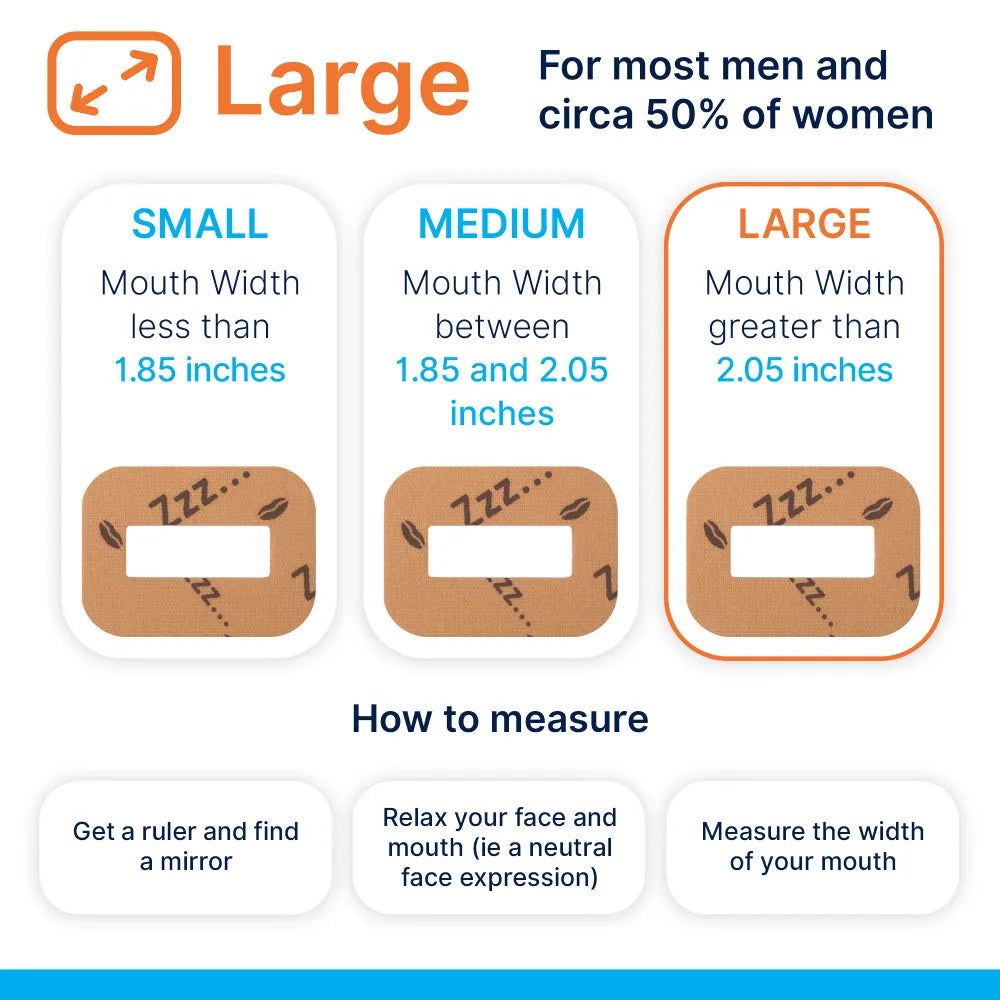
Most mouth tapes seal the lips from edge to edge. Myotape forms a ring around the mouth, creating gentle inward tension that encourages the lips to meet, while leaving a central opening. You can still cough, speak, or part your lips if needed.
Key design points:
- Elastic fabric that follows jaw movement
- Hypoallergenic adhesive on the outer border
- Central gap to reduce feelings of being sealed in
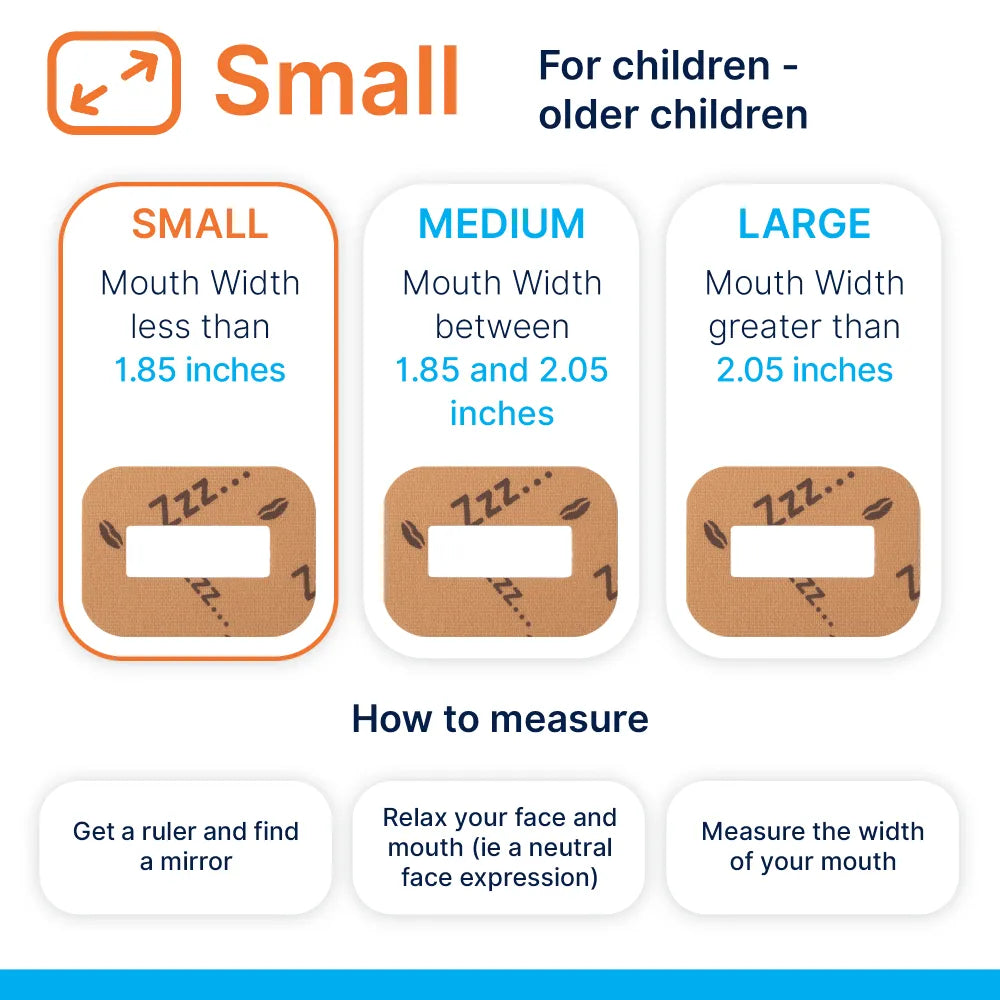
- Sized strips for adults and children, used with care in paediatric cases under clinical guidance
For many, that design lowers anxiety about taping, which can improve adherence during a trial period.
A quick primer on sleep apnoea
Obstructive sleep apnoea, where the throat collapses or narrows during sleep, is distinct from central sleep apnoea, where breathing effort falters. Mouth taping relates to the obstructive form because it addresses airway behaviour and mouth posture.
Severity is often graded by the apnoea hypopnoea index:
- Mild: 5 to 15 events per hour
- Moderate: 15 to 30
- Severe: more than 30
The mainstays of treatment remain continuous positive airway pressure, mandibular advancement devices for suitable patients, weight loss for those carrying extra weight, positional strategies, and targeted therapies for nasal or jaw structure problems. Taping, if used at all, sits in the supportive layer rather than at the centre.
Who might benefit from Myotape
People often report better outcomes with mouth taping when one or more of the following are true:
- Primary snoring without confirmed sleep apnoea
- Mild obstructive sleep apnoea, especially with clear mouth breathing during sleep
- CPAP users who prefer a nasal mask but struggle with mouth leaks
- Those with nasal patency that is good by day but collapses to mouth breathing at night
- Signs of oral breathing habits by day, including dry mouth, frequent gulping, or tongue resting low
It can also be a training prompt alongside myofunctional therapy, which builds lip seal, tongue posture, and nasal breathing habits.
Who should not tape
Safety first. Avoid mouth taping and speak with a clinician if any of the following apply:
- Moderate or severe obstructive sleep apnoea without effective therapy
- Central sleep apnoea
- Significant nasal obstruction, chronic sinus issues, severe allergic rhinitis, or a deviated septum that limits airflow
- Respiratory infection, nausea, vomiting, or a risk of reflux during sleep
- Cardiopulmonary disease where breathing support may be needed
- Skin allergy to adhesives, fragile skin, or recent perioral procedures
- Claustrophobia or panic features worsened by facial coverings
- Children without guidance from a clinician experienced in airway and sleep
If you are unsure, prioritise a home sleep study or lab study first. A short assessment can prevent months of trial and error.
What the research says so far
The evidence base is small but growing. Studies and case series, many in mild obstructive sleep apnoea or primary snoring, indicate:
- Reduced snoring loudness and time spent snoring during the night for some participants
- A drop in apnoea hypopnoea index in selected mild cases, often in the range of a modest improvement rather than full normalisation
- Improved CPAP comfort in nasal mask users through lower mouth leak and less dryness
Research is limited by small samples, short follow up, and varied definitions of responders. That makes careful self‑monitoring essential, ideally with objective data.
Why nasal breathing helps during sleep
Nasal airflow is not just a comfort issue. It changes the airway and gas exchange in useful ways:
- Filtration and humidification reduce airway irritation and dryness
- Nitric oxide produced in the nasal cavity mixes with inhaled air, which relates to better oxygen distribution and may modulate airway tone
- Gentle resistance through the nose can support a steadier breathing rhythm and help keep the soft palate more stable
- Tongue posture improves when the lips are sealed and the mouth stays closed
Some notice less waking to drink water, fewer morning sore throats, and a quieter bed partner. These are good early signs.
Getting started safely
Set aside two weeks for a carefully structured trial. If anything feels wrong, stop and reassess.
Step 1: Check nasal airflow
- Sit quietly and breathe through your nose for five minutes
- If you struggle, address congestion first with saline rinses, allergy care, or medical review
Step 2: Prepare the skin
- Clean and dry the perioral skin
- Trim facial hair where the tape will sit
- Patch test the tape on the forearm for a few hours
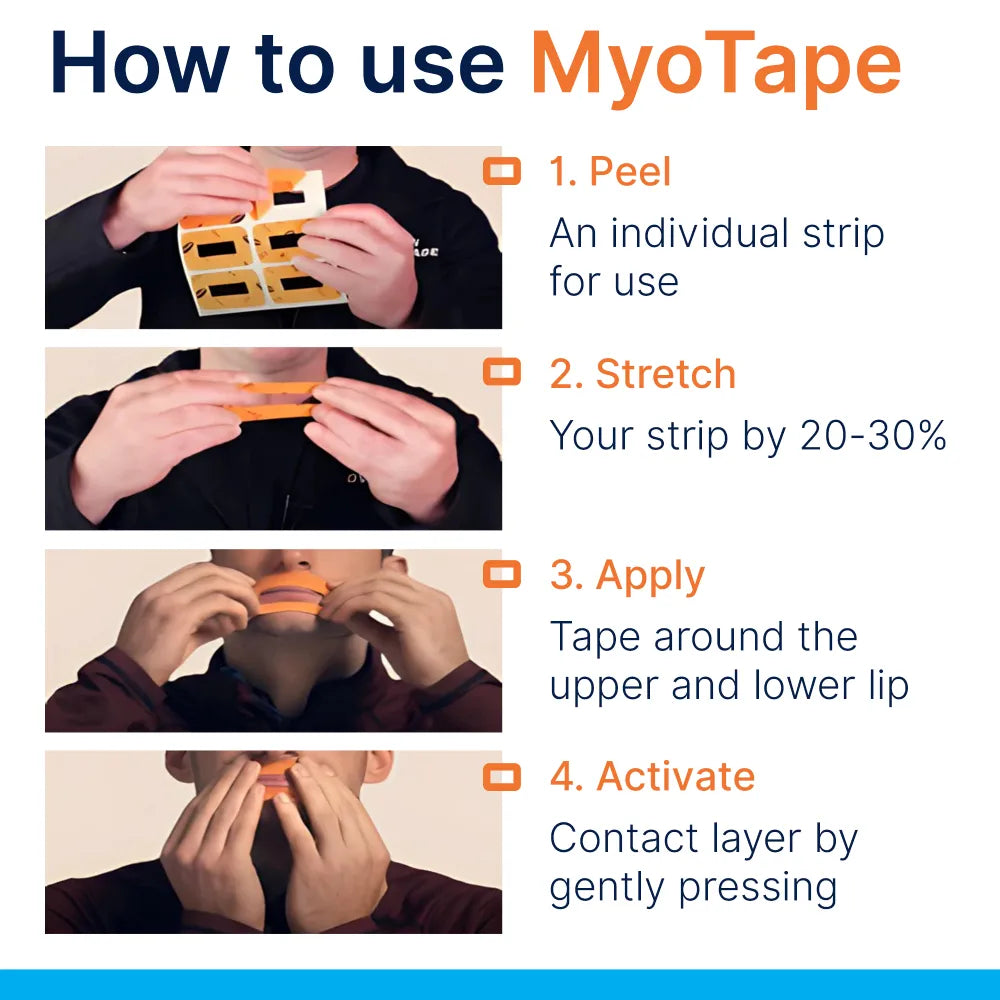
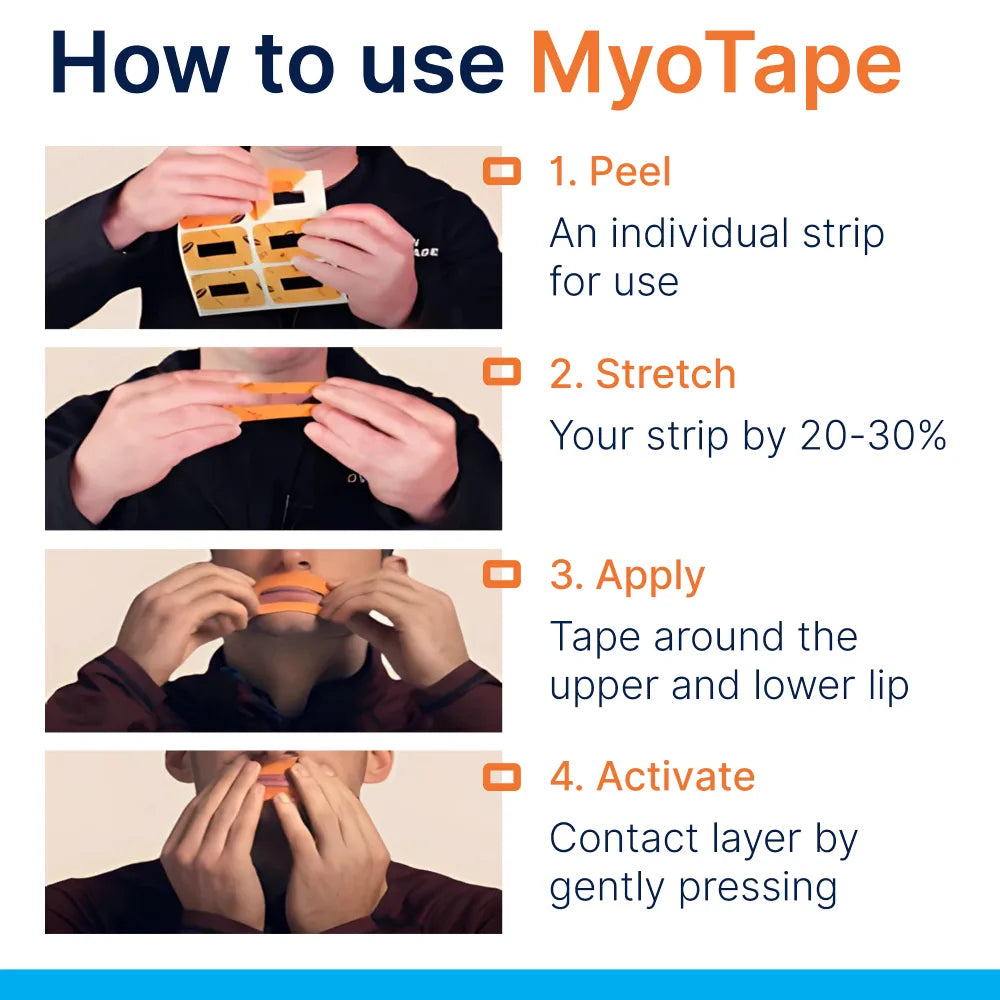
Step 3: Position the tape
- Place Myotape around the lips so the central opening remains free
- The lips should meet lightly, without strain
- You should be able to part the lips with a gentle effort
Step 4: Trial while awake
- Wear it for 20 to 30 minutes in the evening while reading or relaxing
- Practise nasal breathing and light tongue suction to the palate
Step 5: First nights
- Begin on a night when you feel well
- Keep small blunt scissors or a quick‑release strategy available
- Consider side sleeping and a slightly elevated head position
Step 6: Review data
- Use a snoring app, wearable, or home pulse oximeter to track trends
- Ask your bed partner for observations
Stop if you feel breathless, panicky, or wake with pronounced discomfort.
Pairing Myotape with CPAP
Many people prefer a nasal cushion or nasal pillow interface to a full‑face mask. Mouth leaks can spoil that plan by dropping therapeutic pressure and drying the throat. Myotape can help by keeping the lips together without sealing the mouth completely.
Tips for CPAP users:
- Check leak metrics on your machine each morning
- Use heated humidification to counteract dryness
- If leaks persist, consider chin support or a different nasal mask shape
- If you need high pressures or often wake with the mouth forced open, a full‑face mask may still be the steadier choice
Discuss changes with your sleep clinic so your compliance data and symptom changes stay on record.
How it compares with other options
| Option | What it does | Typical use case | Pros | Limitations |
|---|---|---|---|---|
| Myotape | Encourages lip seal with central opening | Snoring, mild OSA, CPAP mouth leaks | Less claustrophobic feel, allows quick mouth opening | Not a core therapy, adhesive sensitivity possible |
| Standard lip tape | Seals lips edge to edge | Snoring, mouth breathing | Simple, inexpensive | Fully sealed mouth, higher anxiety for some |
| Chin strap | Supports jaw closure | CPAP users with jaw drop | Reusable, no adhesive | Can push jaw backward, limited effect on tongue position |
| Nasal dilators/sprays | Improves nasal airflow | Congestion, narrow nasal valves | Directly targets the nose | Variable benefit, overuse of decongestants is risky |
| Mandibular advancement device | Moves jaw forward to open airway | Mild to moderate OSA, snoring | Evidence backed, custom devices can be effective | Dental side effects, adjustment period |
| CPAP | Pneumatic splint to prevent collapse | All severities, especially moderate to severe | Gold standard efficacy | Mask comfort and mouth leaks need management |
Building the foundations: daytime habits
Night‑time taping works best when paired with daytime changes that support nasal breathing.
- Tongue posture: rest the tongue against the palate, tip behind the upper front teeth without pushing
- Gentle nasal breathing drills: slow breath in through the nose, quiet breath out, pause a second, repeat for five minutes
- Lip seal practice: lightly hold a paper strip between the lips while doing easy tasks
- Allergy control: treat hay fever, avoid known irritants, rinse with saline after high pollen exposure
- Oral health: address gum inflammation and dry mouth, which can encourage mouth breathing
These are small, repeatable habits that change the baseline position of the jaw and tongue.
Common questions
Is mouth taping safe for everyone? No. The safety list above matters. Start only when your nose is clear and you have ruled out conditions that make taping risky.
Will it fix sleep apnoea? It may reduce events in mild obstructive cases where mouth breathing is a driver. It does not replace CPAP or oral appliances for moderate to severe cases.
What if my nose blocks at night? Treat the nose first. Consider saline rinses in the evening, a short course of steroid spray under medical guidance, or structural assessment if blockage is persistent.
Can I combine Myotape with a mandibular advancement device? Yes. Many users do, particularly if the device dries the mouth. If the jaw device already delivers good results, tape is optional.
What about drooling or skin irritation? Apply a thin layer of barrier cream around but not under the adhesive area, or use a skin‑friendly tape. Rotate positions to reduce irritation. Stop if redness persists.
How will I know if it helps? Track daytime sleepiness, snoring reports, and device data. An at‑home sleep test before and after a two to three week trial provides a clearer picture.
Troubleshooting guide
- Waking with a dry throat: increase humidification, check mask fit if on CPAP, review nasal care
- Feeling short of breath when trying tape: practise while awake, try a smaller tape size with a larger central opening, or stop and reassess nasal airflow
- Tape falls off: clean skin carefully, avoid moisturiser where adhesive sits, consider a fresh strip each night
- Anxiety at lights out: begin with short evening sessions, pair with a calm routine, try box breathing through the nose
- Bed partner reports continued loud snoring: consider positional therapy, weight management if relevant, review for an oral appliance or a sleep study
When to seek professional review
- Loud snoring most nights with witnessed pauses in breathing
- Morning headaches, severe daytime sleepiness, or memory lapses
- High blood pressure, atrial fibrillation, or type 2 diabetes with suspected sleep symptoms
- CPAP adherence below target because of discomfort or leaks
- Unclear nasal blockage that has not responded to simple care
A sleep clinic can tailor therapy and help you avoid months of guesswork.
A practical two‑week template
Days 1 to 3
- Daytime nasal and tongue posture practice
- Evening Myotape trial while awake for 20 to 30 minutes
- Record baseline snoring and symptoms
Days 4 to 7
- Wear Myotape for the first half of the night
- Review data and bed partner feedback
- Adjust nasal care, humidity, and sleep position
Days 8 to 14
- Wear Myotape for the full night if comfortable
- Recheck objective measures
- Decide on next steps with clinician input if available
Quick checklist
- Clear nose, easy nasal breathing by day
- No conditions on the “do not tape” list
- Skin ready, patch test done
- Data plan for tracking change
- Exit plan if it feels wrong
Sleep is a system. Myotape can support that system for the right person, in the right context, and with the right safeguards. The best signal is how you feel in the day and what the data show at night.













0 comments